A progress report is a key document that provides a detailed account of ongoing tasks, goals, and milestones achieved over a specific period. It helps stakeholders track project development,…
continue reading
Download Medical Incident Report Bundle
Medical Incident Report Format
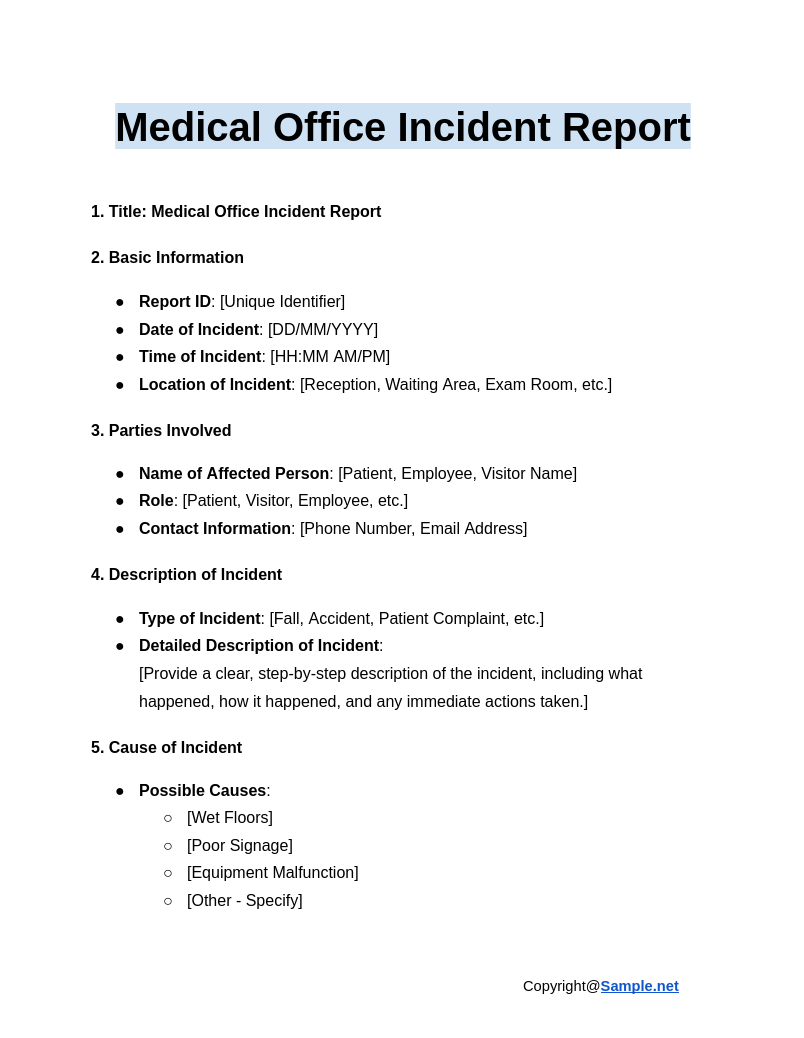
1. Title: Medical Incident Report
2. Basic Information
- Report ID: [Unique Identifier]
- Date of Incident: [DD/MM/YYYY]
- Time of Incident: [HH:MM AM/PM]
- Location of Incident: [Specify Location, e.g., Ward, Room Number, Department]
3. Reporter Information
- Name of Reporter: [Full Name]
- Designation/Title: [Position/Job Title]
- Contact Information: [Phone Number, Email Address]
- Date of Report Submission: [DD/MM/YYYY]
4. Patient Information
- Patient Name: [Full Name]
- Patient ID/Medical Record Number: [Unique Identifier]
- Age: [Age]
- Gender: [Male/Female/Other]
- Ward/Department: [Specify the Department]
5. Incident Description
- Type of Incident: [Medication Error, Fall, Equipment Malfunction, Patient Injury, etc.]
- Detailed Description of Incident:
[Provide a clear, step-by-step description of the incident, including what happened, how it happened, and any immediate actions taken.]
6. Contributing Factors
- Possible Causes/Factors Contributing to Incident:
- [Human Error]
- [Equipment Failure]
- [Communication Breakdown]
- [Other – Specify]
7. Immediate Actions Taken
- Action Taken at the Scene: [First Aid, Medical Intervention, Reporting to Supervisor, etc.]
- Person(s) Notified: [Name, Title, and Contact Information of People Informed]
8. Witness Information
- Name of Witness: [Full Name]
- Designation: [Position/Role]
- Contact Information: [Phone Number, Email Address]
- Statement of Witness:
[Provide a statement from the witness, if applicable, detailing what they observed.]
9. Risk Assessment
- Severity of Incident: [Low, Medium, High, Critical]
- Potential Harm to Patient: [No Harm, Minor Harm, Moderate Harm, Severe Harm, Death]
10. Follow-up and Corrective Actions
- Corrective Action(s) Taken:
- [Changes to Procedures]
- [Employee Training]
- [Equipment Replacement]
- [Other – Specify]
- Person(s) Responsible for Follow-up: [Name, Title, Department]
- Target Completion Date: [DD/MM/YYYY]
11. Recommendations for Prevention
- Preventive Measures:
- [Improved Staff Training]
- [Regular Equipment Maintenance]
- [Updated Communication Procedures]
- [Other – Specify]
12. Signatures
- Prepared by (Name, Title, Date, Signature):
- Name: [Full Name]
- Title: [Position/Role]
- Date: [DD/MM/YYYY]
- Signature: [Signature or Digital Signature]
- Reviewed by (Name, Title, Date, Signature):
- Name: [Full Name]
- Title: [Position/Role]
- Date: [DD/MM/YYYY]
- Signature: [Signature or Digital Signature]
13. Attachments (If Any)
- Photographs: [List any photos attached]
- Witness Statements: [List of attached witness reports]
- Other Relevant Documents: [Medical Records, Maintenance Logs, etc.]
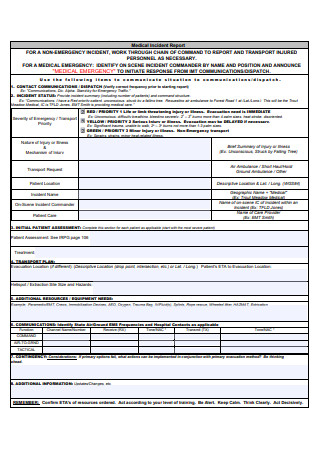
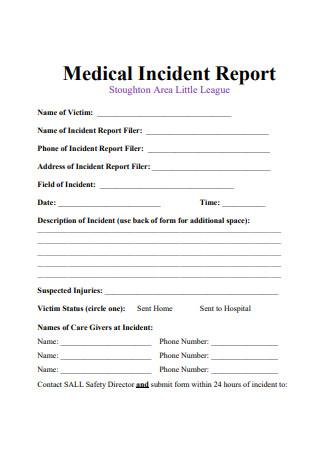
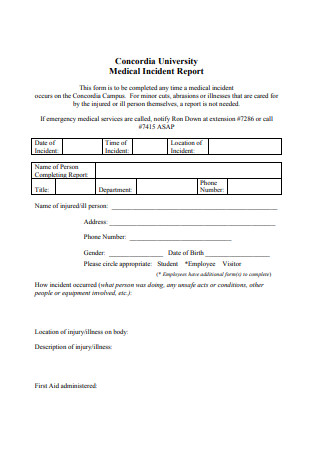
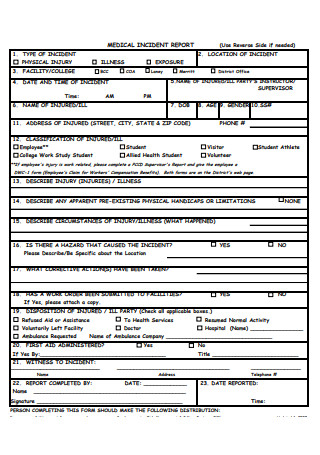
Medical Incident Report Samples
-
Medical Office Incident Report
download now -
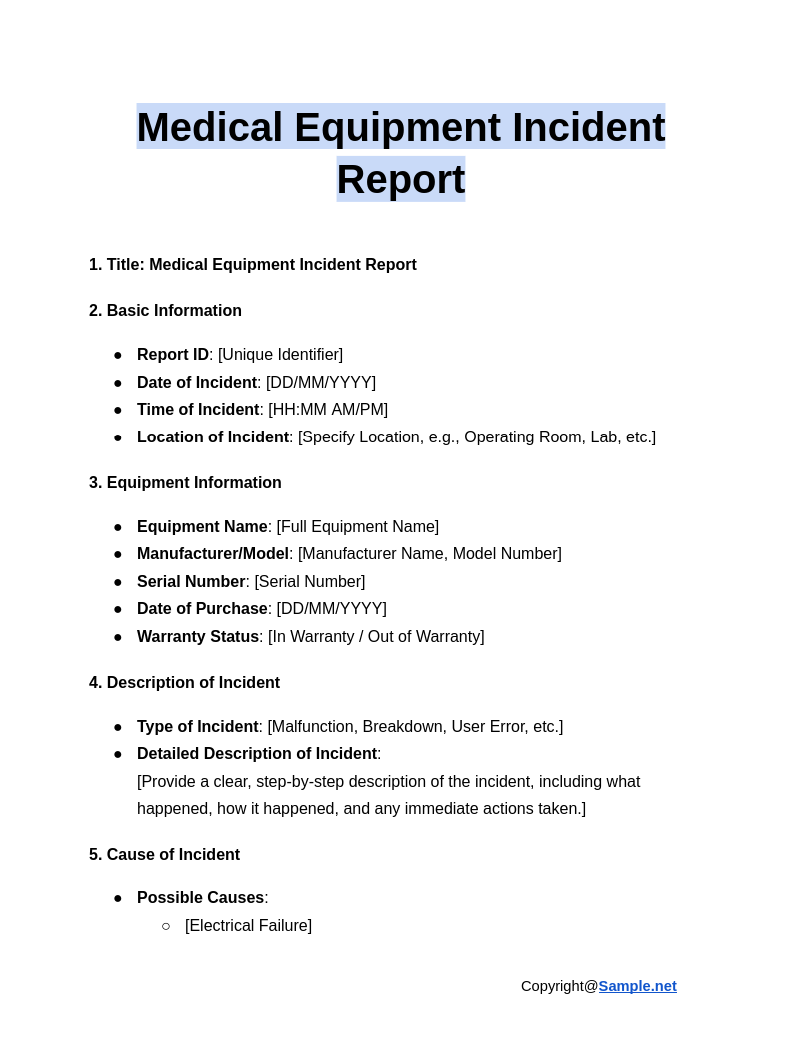
Medical Equipment Incident Report
download now -
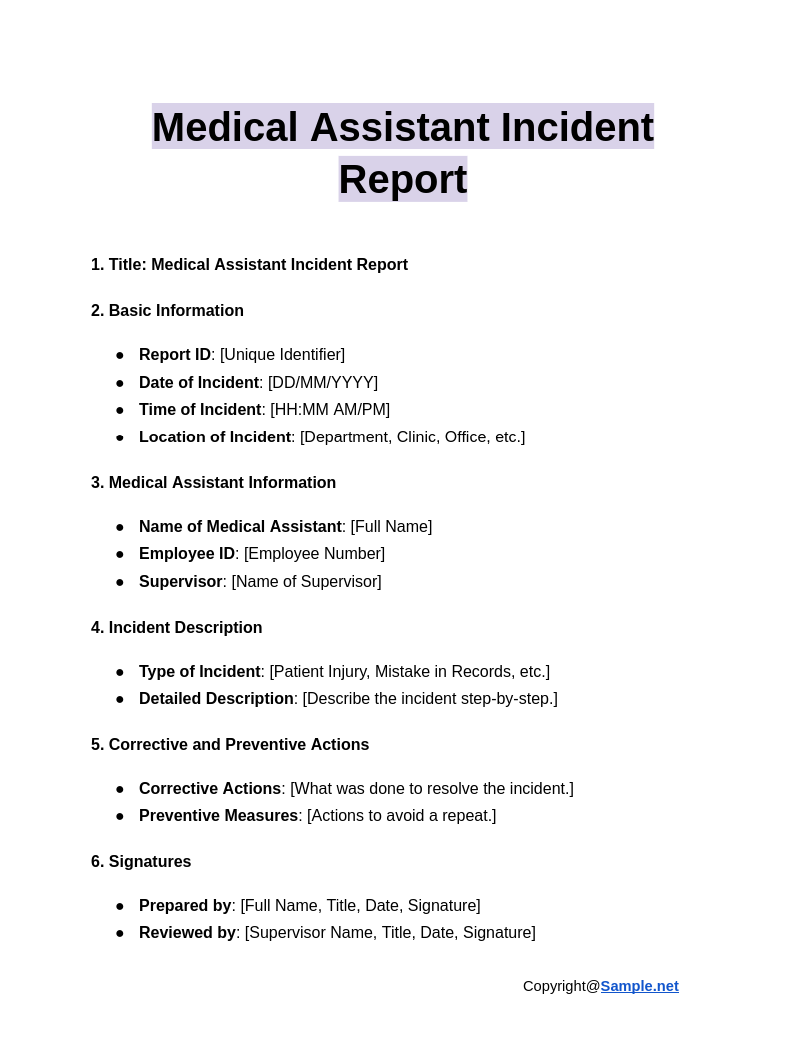
Medical Assistant Incident Report
download now -
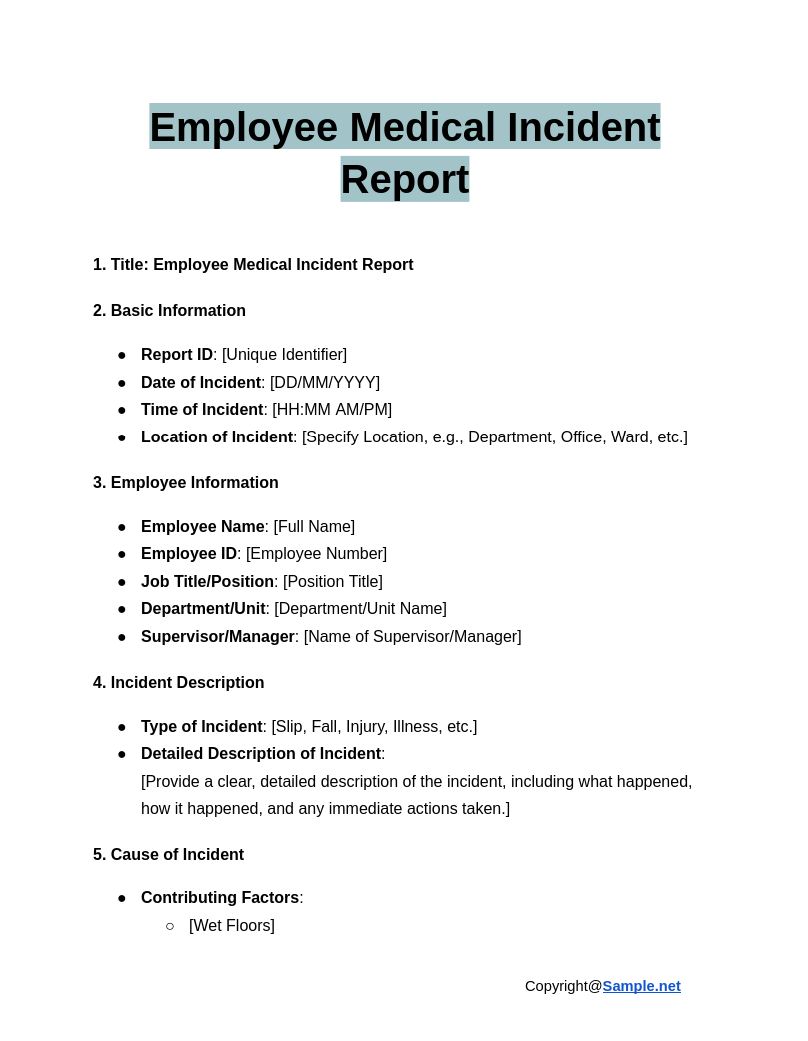
Employee Medical Incident Report
download now -
Medical Incident Report Template
download now -
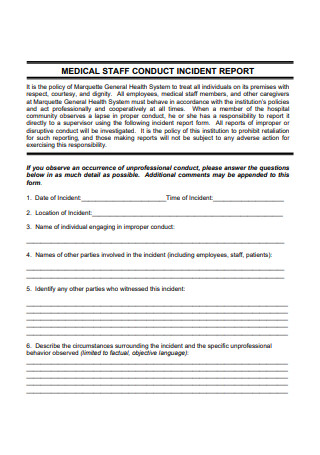
Medical Staff Incident Report
download now -
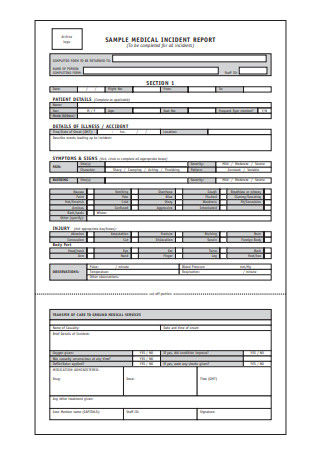
Sample Medical Incident Report
download now -
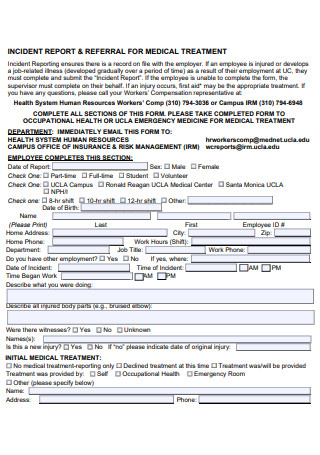
Medical Treatment Incident Report
download now -

Medical Incident Report Example
download now -
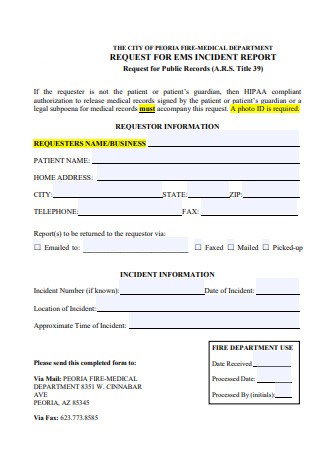
Fire Medical Department Incident Report
download now -
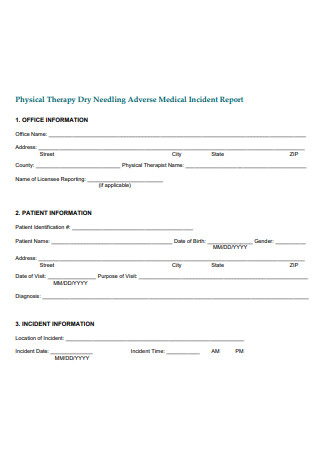
Physical Therapy Medical Incident Report
download now -
Medical Incident Report in PDF
download now -
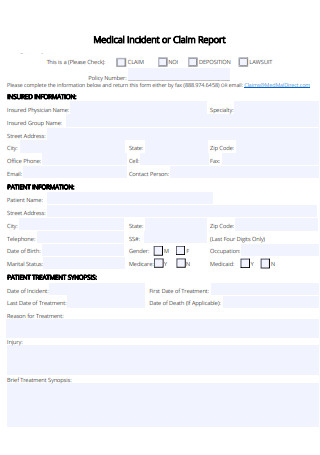
Medical Incident or Claim Report
download now -
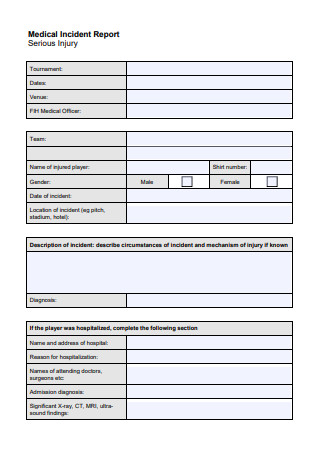
Serious Injury Medical Incident Report
download now -
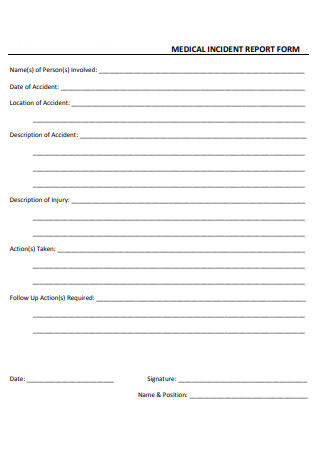
Medical Incident Report Form
download now -
Standard Medical Incident Report
download now -
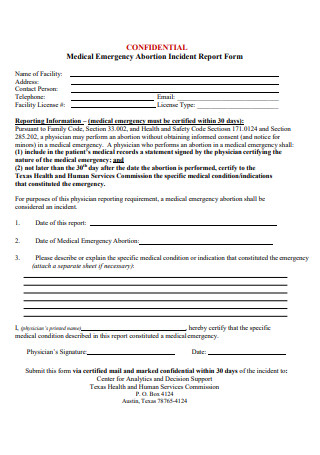
Medical Emergency Incident Report
download now -
Medical Incident Report Format
download now -
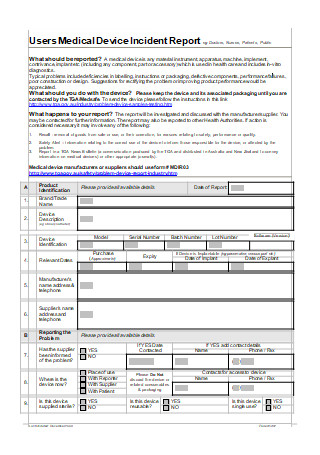
Medical Device Incident Report
download now -

Medical Control Authority Incident Report
download now
What is a Medical Incident Report?
A medical incident report is an accurate, clear, timely, and well-detailed report that provides sufficient information on the chain of circumstances or events that led up to an adverse event that unexpectedly occurs in a healthcare establishment like a clinic, hospital, aging care service facility, ambulatory care facility, and mental health institution. It is a critical communication tool that helps hospital staff members such as nurses, physicians, pharmacists, medical secretaries, and other hospital employees, as well as family members, patients, visitors, and many others to identify and record the root causes of the incident such as communication issues, improper medical procedures, or insufficient staffing. Structuring this report is vital so that the clinicians and medical managers are able to investigate the medical incident and maintain records as references. You can also see more on Patient Incident Report.
Different Types of Medical Incident Reports
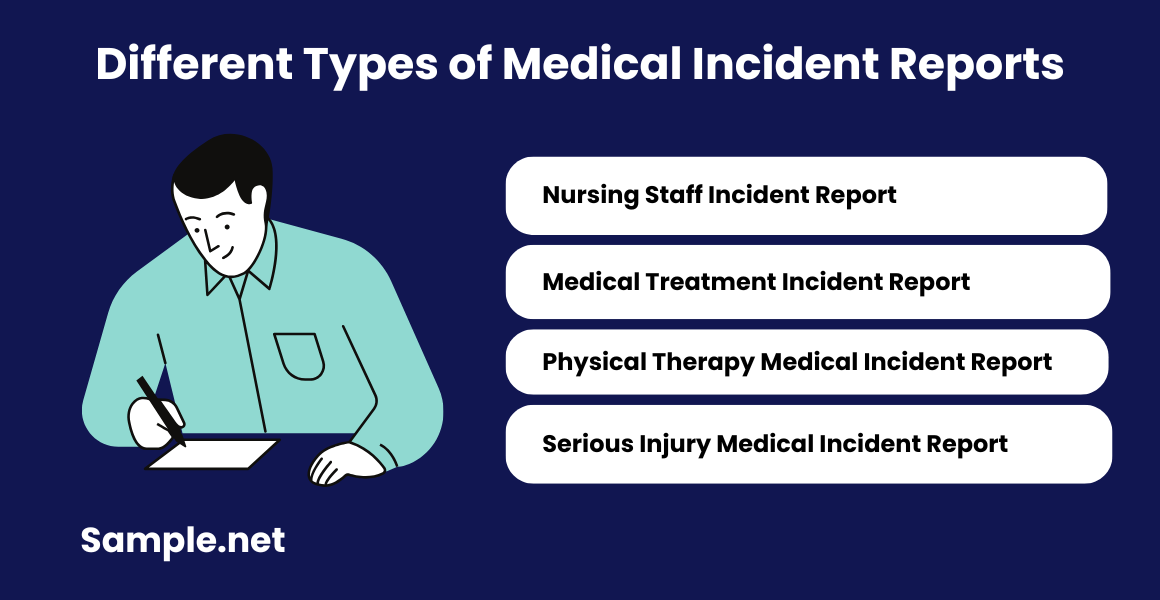
There are wide-ranging types of hospital and traffic incident report forms out there that are used by many clinicians, nurses, physicians, other healthcare staff members, management personnel, and individuals involved in a medical incident. Be knowledgeable about the different types of medical incident reports so that you can be effective in filing medical errors and problems to improve patient safety.
1. Nursing Staff Incident Report
A nursing staff incident report is a type of medical incident and nursing report that must be filed when a nurse or any member of the hospital community observes a lapse in proper conduct within the healthcare facility. The occurrence of unprofessional conduct must be reported directly to a supervisor using an incident report form. All medical incident reports of improper or disruptive conduct submitted by the nursing staff or other employees in the hospital will be investigated according to the policies of the healthcare organization. It contains important details of the incident such as the date, time, and location of the incident, the name of the individual engaging in improper conduct, the names of the other parties involved in the incident, and the description of the circumstances surrounding the incident and the specific behavior observed.
2. Medical Treatment Incident Report
Incident reporting for medical treatment ensures there is a record on file with the employer. If an employee is injured or develops a job-related illness that gradually developed over a certain period of time as a result of their employment at the company, they need to complete and submit the medical treatment incident report. If the employee is unable to fill up the medical incident form, the supervisor should fill up the document on their behalf. Typically, it contains information about the employee such as the full name, home address, home phone number, work hours and shift, department name, job title, work phone number, other employment details if applicable, date and time of the incident, and the description of what the employee is doing and all injured body parts. Also, take note of the initial medical treatment provided. You can also see more on Preliminary Incident Report.
3. Physical Therapy Medical Incident Report
A physical therapy medical incident report is completed on the patient of physical therapy to indicate a specific incident that took place. For example, physical therapists use therapeutic dry needling to treat pain and increase the range of motion in injured patients. When it is performed improperly or in an unsterile manner, there are possible risks and side effects that can cause serious and life-threatening harm such as extensive bruising, severe nausea, vomiting, pneumothorax, and puncture of other vital tissue or organ. For this report, outline the office information, patient information, and incident information.
4. Serious Injury Medical Incident Report
A study conducted in California focused on ameliorable adverse outcomes or adverse outcomes due to negligence to patients in the course of health care management and reported 4.65 injuries to patients per 100 hospitalizations. Also, subsequent studies have consistently found that 10%-12% of patients experience harm while hospitalized. When medical incidents led to serious injury, it is important to make an accurate medical incident report. Describe the circumstances of the incident and the mechanism of injury if known. You can also see more on Medical Report.
Benefits of Medical Incident Reports
Healthcare staff tends not to report mistakes or near misses because they fear that if they do, they will be blamed and punished. However, incident violation report of medical accidents and other issues is fundamental to set up effective procedures which act as barriers to prevent mistakes. Also, senior staff and clinical management must trust the team to exercise due vigilance, attend training, and report issues when they happen.
How to Write a Medical Incident Report
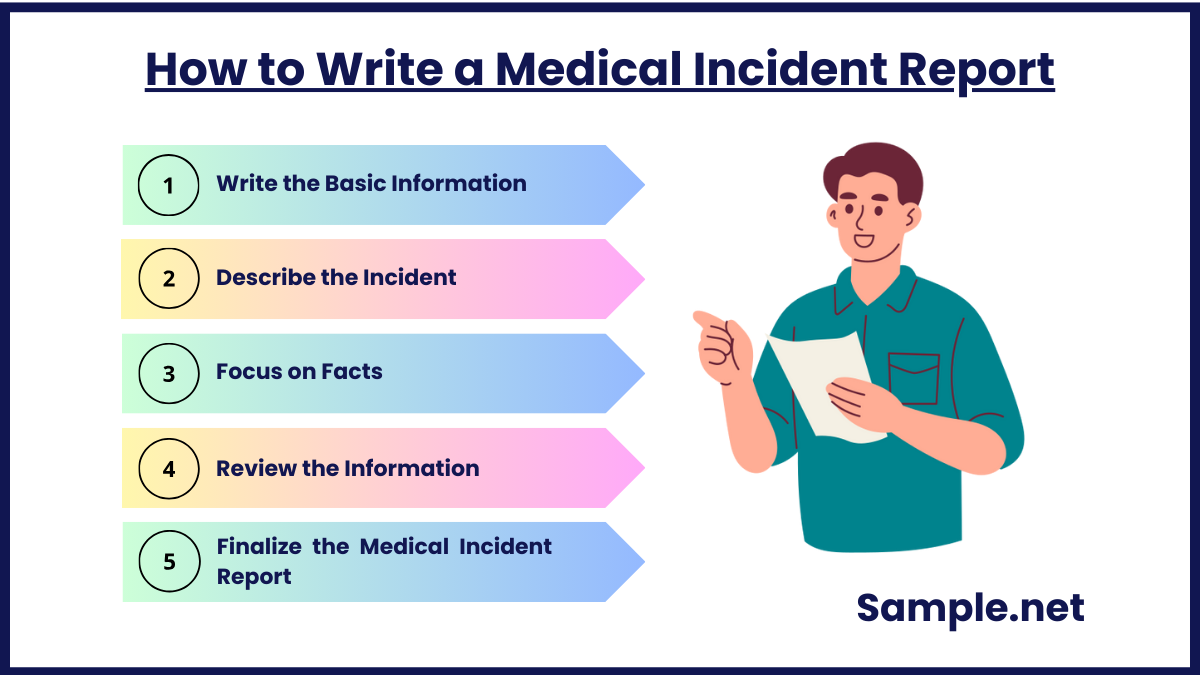
A national health institution believed that a serious adverse event or critical medical incident takes place in up to 10% of all hospital admissions, which means about 850,000 adverse events per year. Those incidents cost billions every year in increased hospital costs, treatments, and litigation. Despite the difficulties in the healthcare and medical sector around the world, it is integral for healthcare providers and individuals to use a medical incident report along with a health and safety audit checklist to have the best insight into whether certain processes are actually working and prevent risks.
Step 1: Write the Basic Information
The needs for incident reporting for healthcare and medical institutions may vary by organization. But writing the basic information regarding the person involved in the incident is generally required. Include the name of the patient, date of birth, hospital ID number, names of any other affected individuals like staff or visitors, date, time and location of the incident, name, and address of the medical facility where the incident happened, and the type of incident (e.g., equipment failure, medication error).
Step 2: Describe the Incident
Create a short and factual description of the incident. It must be written in chronological order. Identify the name of the witness and their contact details such as cellphone number and email address. Add the details and total cost of the damage or injury, if any. Define the action taken at the time. Then, include the name of the physician or the medical staff who was notified of the incident and the name and contact details of the person reporting the incident. You can also see more on Laboratory Incident Report.
Step 3: Focus on Facts
The medical incident report should aim on presenting clear facts. Provide comprehensive details of your direct observations, actions taken, the provided assistance, and communications. Describe specifically what you saw when you arrived on the scene or what the witnesses noticed from the incident. Add direct quotes and statements from the patient and other parties involved in the event.
Step 4: Review the Information
After describing the incident, review the information you included in the medical incident report. Skim the document and see if you forget important details that should be displayed in the report. Edit and revise the report immediately as you add all the core points of the incident.
Step 5: Finalize the Medical Incident Report
Check the format and outline of the medical incident report. After proofreading and revision of your document, you can now finalize the medical incident report. You can use manual or electronic incident reporting using incident management software available in your healthcare facility.
A Medical Incident Report plays a vital role in enhancing patient safety, accountability, and healthcare quality. Proper documentation enables medical facilities to learn from past incidents, avoid future risks, and maintain high standards of care. Effective reporting fosters a proactive approach to health and safety in medical environments. You can also see more on Audit Incident Reports.
FAQs
Some examples of medical incident reports are medical school incident reports, medical nursing staff incident reports, employee medical incident reports, patient medical incident reports, medical work incident reports, medical emergency incident reports, medical treatment incident reports, fire medical department incident reports, physical therapy medical incident reports, and serious injury medical incident reports.
The common types of incident reports are workplace incident reports, accident or first aid reports, safety and security incident reports, and exposure incident reports.
When writing an incident report in healthcare, specify the name of the patient, hospital number, and date of birth. Indicate the date, time, and location of the incident. Add a brief and factual description of the incident. Also, include the name and contact information of any witnesses. Describe the harm caused, if any and the action performed at the time. You can also see more on Incident Analysis Reports.
The purpose of a medical incident report is a beneficial document included in a health and safety coordination plan. It draws attention to a specific incident to prevent future incidents or lower the likelihood that future incidents will take place.
Creating a medical incident report is important because it aims to improve patient safety and care quality. It is a crucial report that identifies safety hazards and guides the development of interventions to mitigate risks in order to reduce harm. Plus, it assists the staff in determining and modifying the individual or system-level factors related to medical errors.
What are some examples of medical incident reports?
What are the common types of incident reports?
How to write an incident report in healthcare?
What is the purpose of a medical incident report?
Why is creating a medical incident report important for healthcare organizations?