10+ Sample Nursing Incident Report
-

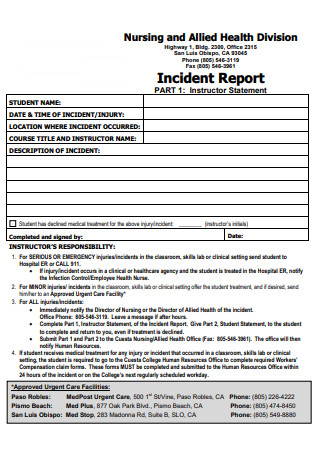
School of Nursing Health Incident Report Form
download now -
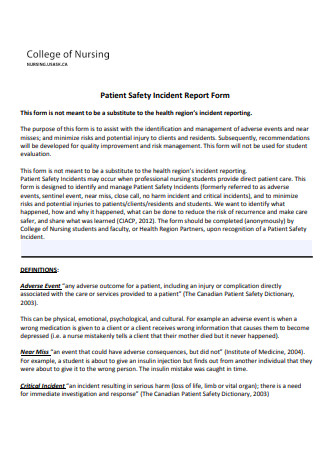
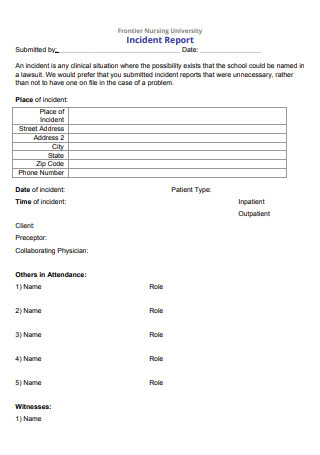
College of Nursing Patient Safety Incident Report Form
download now -
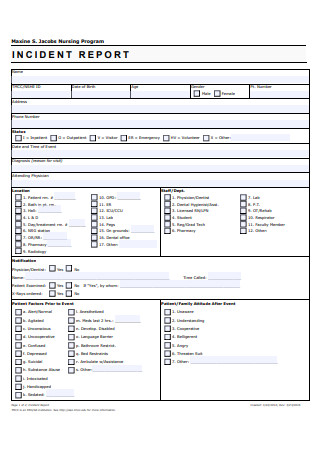
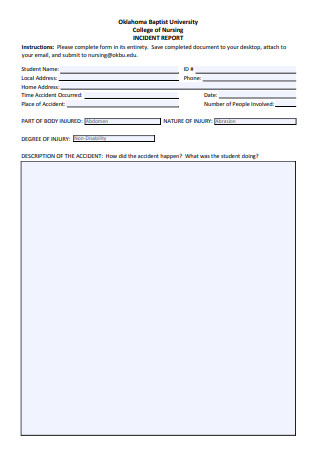
Nursing Program IIncident Report
download now -
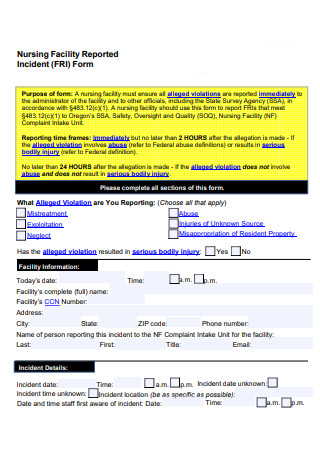
Nursing Facility Incident Reported Form
download now -
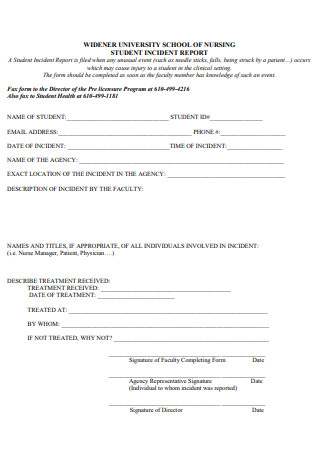
Nursing Student Incident Report
download now -
Nursing Incident Report Example
download now -
Basic Nursing Incident Report
download now -
College of Nursing Incident Report
download now -
Nursing Incident Report in PDF
download now -
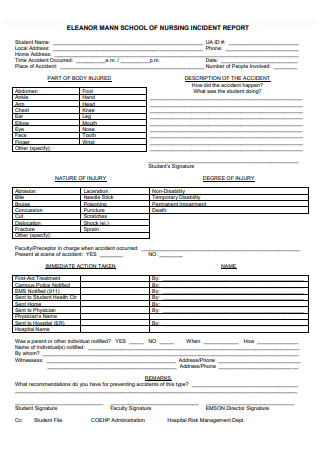
School of Nursing Incident Report
download now -

Printable Nursing Incident Reporting
download now
FREE Nursing Incident Report s to Download
10+ Sample Nursing Incident Report
What Is a Nursing Incident Report?
What Are the Information Needed in a Nursing Incident Report?
What Is the Desired Outcome of Writing a Nursing Incident Report?
What Is the Difference Between a Nursing Incident Report and Medical Incident Report?
Purpose of a Nursing Incident Report
How to Write a Nursing Incident Report
FAQs
What to Expect After Writing an Incident Report?
What Do I Need to Tell the Patient and the Patient’s Family?
Do you dread writing a nurse incident report?
What Is a Nursing Incident Report?
A Nursing Incident Report is a document may it be a paper or a typewritten one that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side. This kind of report is not only limited to causing harm to a patient, employee, or even visitor but it can be any unseen event, incident, or accident that threatens the safety of the patient inside a facility or outside. All details or sequence of events must be accurate as possible and incident reports should be complete within twenty-four (24) hours, unlike the laboratory incident report that should be completed and submitted within forty-eight (48) hours after the incident has occurred.
Nursing incidents do not happen only in the hospital facility but also at home. We have another form of report which is called a nursing home accident report where it is also a document that sums up the sequence of events that happens in a nursing home and not just merely inside hospital premises. If in an instance that the accident or incident was not observed or nobody saw it just like a patient falling but was able to stand up on his own, the first hospital personnel who was immediately notified should submit the incident report having all the detailed information and sequence of the events from the patient.
What Are the Information Needed in a Nursing Incident Report?
An incident report should be completed every time that an accident or any mishaps in giving care to the patient or any instances or possibilities of deviating from the normal operation and routine of the facility and/or from the patient. The necessary information that is vital in a nursing incident report should have a comprehensive and detailed sequence of unknown events. The document information may vary but it typically includes the people who witnessed such incident, more like the person who reported the incident although there are some cases that there are more witnesses covered in the setting. Another thing to consider and is necessary in the nursing incident report is the casualties or any person who was involved or in pain, like for example a patient, a significant other, or even a nurse. Next are the persons who were notified like the treating physician, the emergency personnel, or the administration. The actions or interventions are also necessary for the nursing incident report as this can be used for the investigation of what happened on the scene. All events that happened during the scene of the accident should be listed chronologically as well as the contributing factors. Recommendations for change can also be essential in the nursing incident report for the prevention of future incidents or accidents.
What Is the Desired Outcome of Writing a Nursing Incident Report?
In writing an incident report a positive outcome should always be manifested but that depends on the event of the accident. There are times that the outcomes are deviated from what we expect and manifest. For pessimistic situations that will not happen in the future, a good, desired outcome must be manifested in writing a nursing incident report. The desired outcome of writing an incident report is to document the occurrence or happening of an unexpected event that involves the physical or psychological aspect of injury to a patient, visitor, significant other, employee, and even healthcare professionals or that increases the risk for injury. Furthermore, the desired outcome is to identify changes that need to be made in the facility to prevent the recurrence of such events and promote overall safety and quality health care to all personnel in the hospital facility.
What Is the Difference Between a Nursing Incident Report and Medical Incident Report?
Incidents happen from time to time. We cannot deny the fact that accidents of different kinds may occur or happen unexpectedly. Such cases may happen inside a hospital facility. It can happen in the operating room, wards, nurses’ station, laboratories, and even emergency rooms. Emergency rooms are somewhat more susceptible to different kinds of accidents since all personnel inside this room are always in a hurry. The tendency of always being in a hurry is that it is very prone to accidents such as spills, leaks, falls, or even a mix-up of medications given to the patients. The reason for this is that most people go directly to the emergency room to seek care.
Emergency personnel often do a triage if the person is really exhibiting the correct signs and symptoms of a specific disease or illness. When accidents happen, an incident report is being written for the higher administration to investigate it and to render continuous care to the patients. When we say a nursing incident report, it provides detailed information and a sequence of events that happens when a nurse is present. Or when there is a deviation from safe nursing standards. On the other hand, a medical incident is an event where it happens usually to other healthcare professionals like the doctor, dentists, physical therapists, and so on. Although they have are their own incident report form depending on the field that they are working in, it will still not change the fact that incident reports should be made by different fields of medicine. A medical incident report’s intention is to establish control of the accident, have a systematized process for reporting any medical injuries, and enable any health professionals to transmit and convey information.
Purpose of a Nursing Incident Report
Nursing incident reports are used to initiate communication in sequencing events about the important safety information to the hospital administrators and keep them updated on aspects of patient care. Writing an incident report has its own purpose that will provide us a clearer understanding of how it works and how it is done. The following purposes of a nursing incident report are stated:
How to Write a Nursing Incident Report
1. Use Clinical Reasoning and Judgment
This is to confirm that an accident or incident has occurred that requires an incident report. Clinical reasoning and judgment must be possessed by a clinical health practitioner or any healthcare professional. It is a skill that is needed to be learned in a span of time. Completing an incident report with this kind of skill even if the result would likely correspond to disciplinary action can help in the creation of a nursing incident report.
2. Meet and Document the Statements
Documenting the statements of the principal parties involved as well as the witnesses to the event can be used in cases where an incident would rule out as negligence. The information from the witnesses and the persons involved in the accident should be obtained from patients, visitors, significant others, or even from the healthcare professionals if applicable. You must arrangements to meet the needs when these people have current ailments or barriers such as illiteracy, language barriers, or deafness. When there is a language barrier between two (2) parties, you may use a professional certified medical interpreter, either in person or via personal call or video call.
3. Input the Necessary Information
Document and put all necessary information such as the identity of the patient, visitor, significant other, or employee. Also, include the location, time, and date of the incident. As well as the names of the persons other than the patient, visitor, significant other or employee who were involved in the incident wherein they can serve as witnesses. You must also include a detailed objective description of the incident, and all necessary statements, actions, interventions, and outcomes.
4. Do Not Include Subjective Information
Subjective information is those details or statements with personal assumptions, conclusions, opinions, or even suggestions in which it can be false information and not an accurate statement. Do not include those statements that have a similar sense wherein the witness or the person involve talks about a similar incident from the past.
5. Do Not Document Incident Report in Patient’s Medical Record
Documentations that are involved in the patient’s medical record are his or her objective findings from the doctor. For example, the assessment, diagnosis, planning, intervention, as well as evaluation. Documenting and writing the incident report are not usually included in the medical record of the patient.
6. Verify the Nursing Incident Report Form and Affix Signature and Data
Checking the nursing incident report can make it more comprehensive in which proofreading helps you to be aware of some mistakes and errors as you are making the incident report. After checking the nursing incident report, you must affix your signature together with your name and the date that you signed the nursing incident report form. After filling out the necessary details and information in the incident report form, it is then submitted to the nurse manager or risk management department according to the hospital facility protocol with the purpose of further investigation of the scene.
Always be aware that incident reports could potentially be used for legal purposes when proven that it is done out of negligence in which providing incomplete, inaccurate, and false information of the incident may give harm to the patients and may jeopardize the defense of any case that may include your own profession. For this to be prevented, you should document everything that happened. It is taught in nursing school that any situation or anything that is not documented has not been done or did not happen and occur, so it is best to document accurate data.
FAQs
What to Expect After Writing an Incident Report?
Information in the nursing incident report will be analyzed and comprehended to identify the root cause of the incident. This is subject to changes that need to be made in the facility or to facility processes to prevent recurrence of the incident and promote overall safety and quality of care.
What Do I Need to Tell the Patient and the Patient’s Family?
Educate the patient or the significant other on what to expect regarding the incident report. Impart an explanation when results of some procedures are given in association with the condition of the patient or visitor.
Do you dread writing a nurse incident report?
Now, that depends on the person writing it. Stressing over getting the report done or about what to include are common concerns for nurses. Always take into consideration that if you will write a nursing incident report, you should not be biased about it but instead you should write it truthfully and with an honest heart.
Incident Report format may depend on the organization and the practice setting. Regardless of whether you are a nurse or any other medical practitioner, you should always hold the responsibility to adhere to and follow the incident reporting guidelines that are established by your facility. There are a lot of free incident report templates published online, you may access them if your institution does not require any formats. But it is a big doubt if your institution or hospital does not follow any guidelines in making and writing an incident report.
