50+ Sample SOAP Notes
-

SOAP Note for Chronic Problems Example
download now -

School of Pharmacy SOAP Notes
download now -

SOAP Notes Templates
download now -

Patient Assessment SOAP Note
download now -
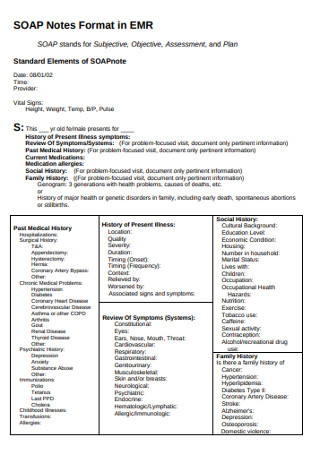
SOAP Notes Format
download now -

Student SOAP Note
download now -
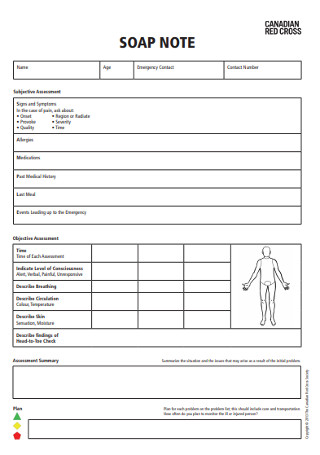
Red Cross SOAP Note Template
download now -

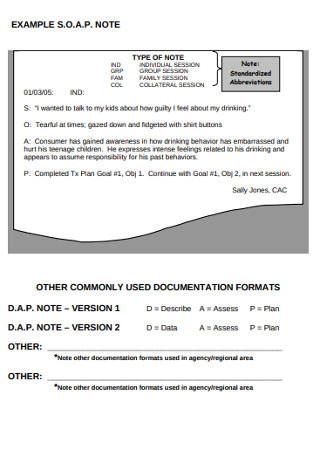
Standardized SOAP Notes
download now -
Sample SOAP Notes
download now -
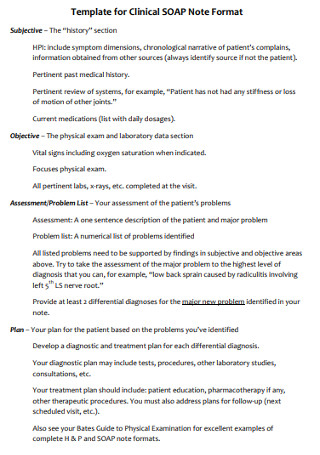
Template for Clinical SOAP Note Format
download now -

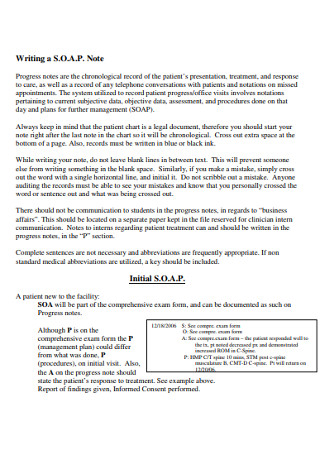
SOAP Progress Notes
download now -

SOAP Note Plan Examples
download now -

Daily SOAP Note Example
download now -
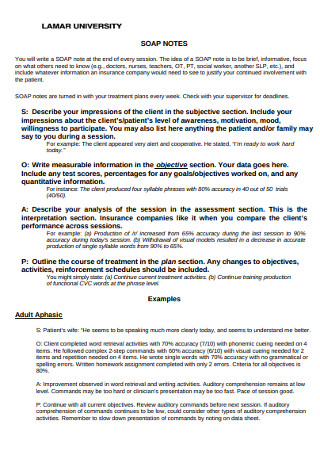
University SOAP Note Template
download now -
SOAP Counselings Note
download now -

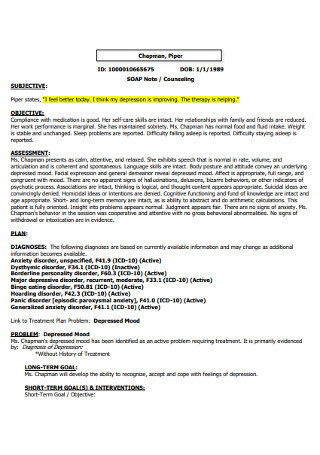
Psychiatry Follow-up SOAP Note
download now -
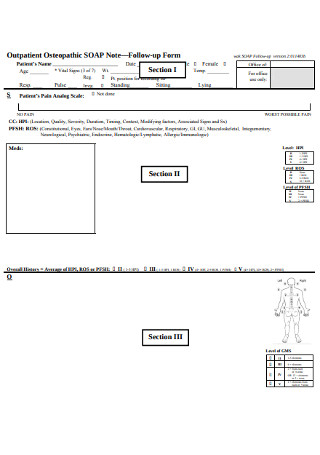
SOAP Note Follow-up Form
download now -

Routine SOAP Note Example
download now -

Graduate SOAP Notes
download now -
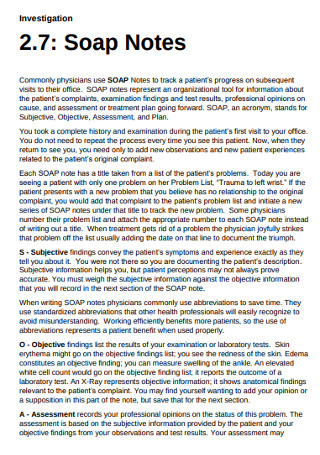
Investigation Soap Notes
download now -
Basic SOAP Note Example
download now -

Diagnosis SOAP Note
download now -

Inspection SOAP Note Template
download now -

Sample Narrative SOAP Note
download now -

SOAP Note Documentation Template
download now -

SOAP Model for Recording Session Case Notes
download now -

Student Academic Learning SOAP Notes
download now -
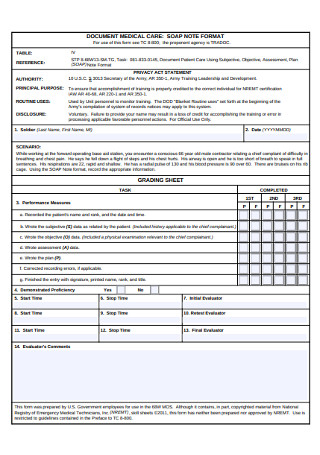
Medical Care SOAP Note
download now -
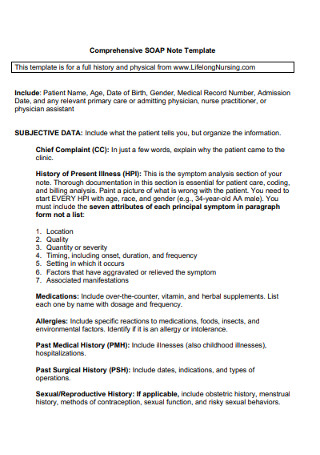
Comprehensive SOAP Note Template
download now -

Sample Pulmonology SOAP Note
download now -
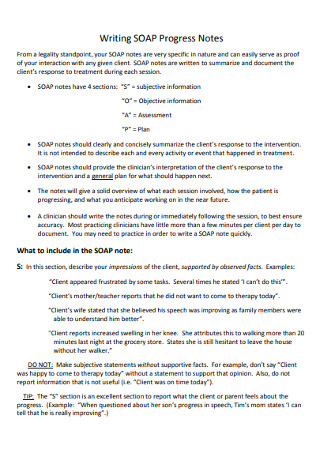
SOAP Progress Notes Example
download now -

Financial SOAP Note
download now -
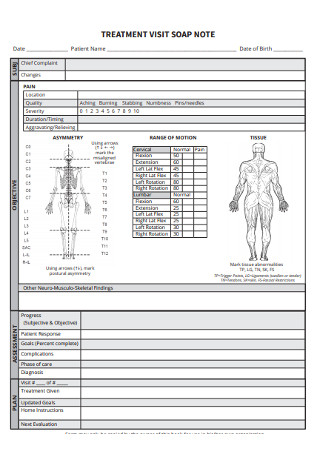
Treatment Visit SOAP Note
download now -
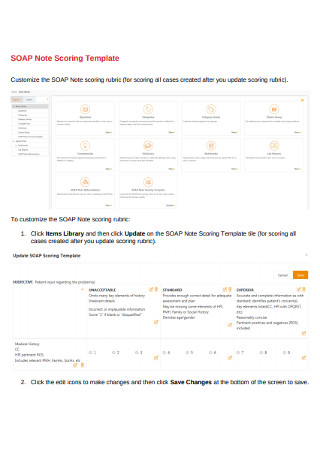
SOAP Note Scoring Template
download now -
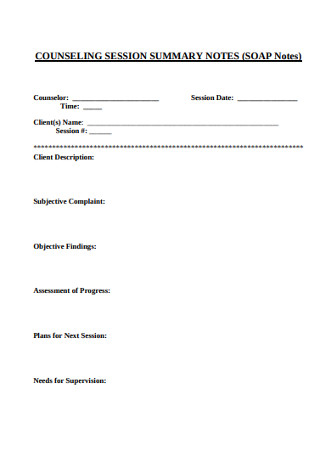
Counseling Session Summary SOAP Notes
download now -
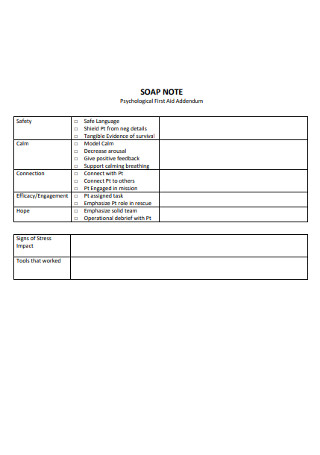
Psychological SOAP Notes
download now -

Nutritional Supplement with SOAP Notes
download now -
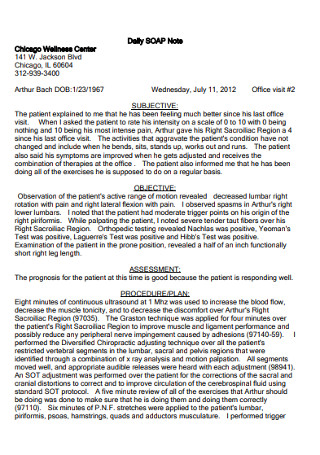
Daily SOAP Note
download now -
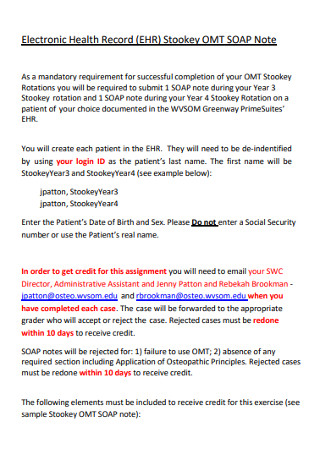
Electronic Health Record SOAP Note
download now -
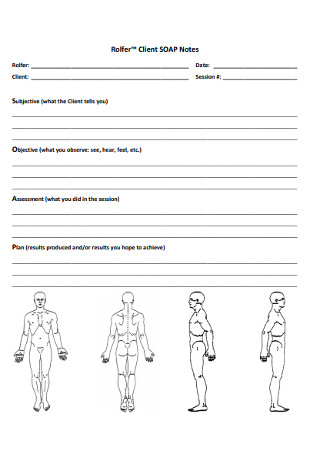
Client SOAP Notes
download now -
Ethics and Law SOAP Notes
download now -
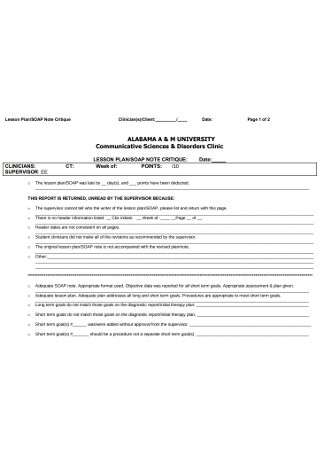
SOAP Lesson Plan Notes
download now -

Patient SOAP Note Charting Procedures Example
download now -
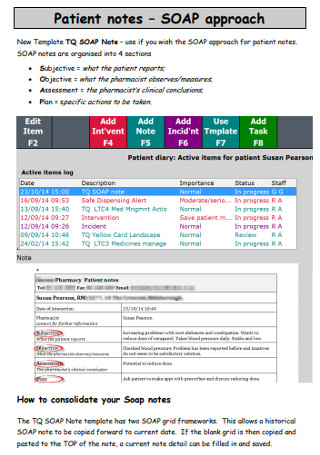
Patient SOAP Approach Notes
download now -
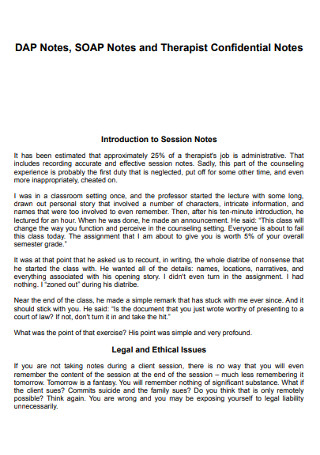
SOAP Notes and Therapist Confidential Notes
download now -
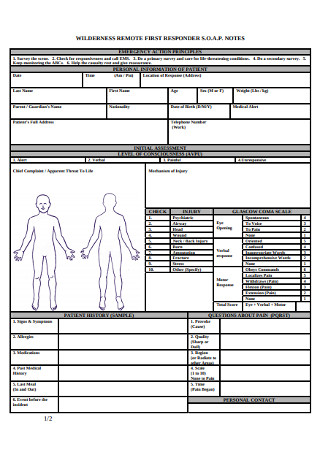
Wilderness Remote First Responder SOAP Notes
download now -
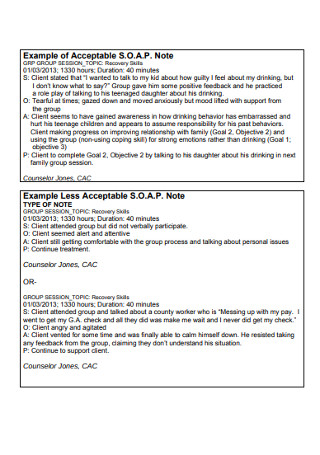
Acceptable SOAP Note Example
download now -
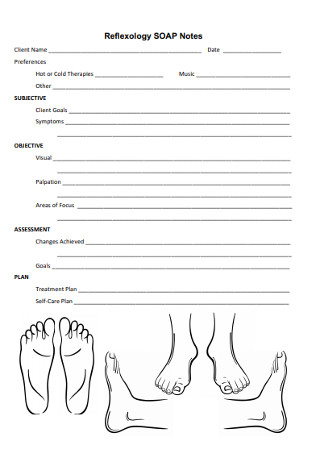
Reflexology SOAP Notes
download now -

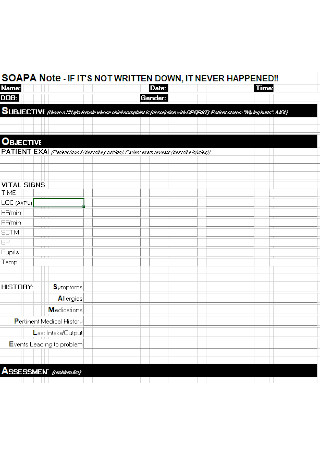
Standard SOAP Note Template
download now -

SOAP Notes and Progress Notes
download now -
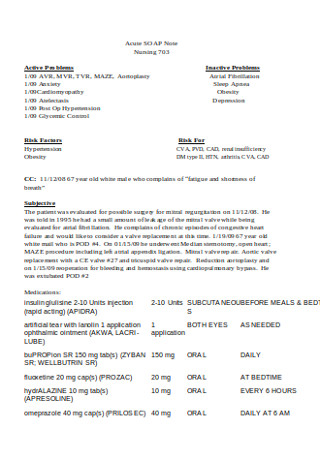
Acute SOAP Note Template
download now -
Bsic SOAP Note Example
download now
What Is a SOAP Note and What are Its Components?
To understand a SOAP note, we have to go way back to when Dr. Lawrence Weed first introduced it to the world of medicine in the 1960s, when it was then known as the Problem-Oriented Medical Record (POMR). It enabled physicians to handle complex patient cases in a structured manner to help standardize the process for other professionals in the field. Since then, various disciplines began utilizing its “SOAP” format for medical documentation instead, which is why you won’t find a lot of practitioners adopting the POMR anymore.
A SOAP note is basically a method of documentation that medical professionals employ to record a patient’s progress during treatment. Health care providers can use it to communicate the status report of a patient to other practitioners, giving them a cognitive framework that they can refer to, upon assessment.
There are four components of the note, namely:
Subjective
Upon medical consultation, patients provide a brief statement about their purpose for visiting. The chief complaint may relate to how a patient has been feeling and what they believe could have caused the discomfort. The physician may also ask a few questions to find out what the problem is in connection with the patient’s narrative. Keep in mind that every case is different. What one would describe as the most painful feeling could only be a moderate experience to another.
Objective
In this section of the SOAP note, the physician makes objective observations on the patient, which may include results from a physical exam, lab report, diagnostics test, and the like. The objective component of the note can also discuss what the doctor can measure from the patient’s current state. Everything listed must be factual, which means that additional documentation may be necessary to support the data written in the note.
Assessment
This part of the SOAP note defines the condition that the patient has, which may or may not include a diagnosis. It is common for a physician to list more than one possible diagnosis in the note, especially if there isn’t enough evidence to rule out the others, so there’s no reason to worry. Doctors may also identify drug-related or -induced problems as a possible cause for the symptoms experienced by the patient.
Plan
As for the last part of the SOAP note, the physician will write down actionable items to address the patient’s problem. It may involve further testing, prescribed medication, or simple home remedies to help the patient recover on their own.
Why Use a Soap Note?
There are good reasons why medical and behavioral health professionals around the world continue to rave about the SOAP format. But among the countless benefits that a SOAP note has to offer to those who use it, here are our top three:
Paper Charts vs. Electronic Medical Records: Which Is Better?
Hospitals, clinics, and health care facilities around the world are doing their part for the environment by implementing a paperless system. Today, you can find many medical professionals using an electronic medical record (EMR) to capture and share patient information for experts in their practice to use. It serves as an alternative to paper charts or tracking charts that often fill the records room of a hospital.
But there continues to be a debate on whether electronic records can replace paper records in the near future.
In terms of which type of record is the most efficient, the answer to that question would depend on the resources available and whether the user is computer literate enough to rely on an EMR system to store patient information.
How to Write a SOAP Note: Tips to Remember
Among the 1.1 million physicians in the United States, 160,000 of which are inactive, and another 55,000 are marked unclassified in a report made by Statista. If you analyze these figures and the number of individuals that require medical assistance each day, you can tell how much work medical practitioners have to go through to attend to the needs of the general public. Fortunately, streamlining this process with the help of a SOAP note is one way to ensure that patients get the best possible treatment and care from their attending clinicians, while also giving these doctors the convenience of having an organized record.
But for these progress notes to be useful, there are certain matters to be mindful of when creating a SOAP note.
1. Subjective: Gather Information
Interview the patient. You can ask how they’re feeling or what symptoms they’ve been experiencing recently to find out what to consider in your treatment plan. Collect as much information as possible based on what the patient can tell you about their condition. While you can never rely on a nonmedical professional’s prognosis, you have to agree that no one knows their body more than themselves. That is why you must document the patient’s own words to keep insights about their condition completely accurate. You must also take a patient’s personal or medical issues into account, as this may also play a part in their performance plan.
What to Avoid: Refrain from adding comments that lack supporting evidence. Your planning statements will remain an opinion until you have enough facts to prove otherwise, which is why it’s best to include only what is relevant to the case to avoid problems down the line.
2. Objective: Make Observations
Although a patient’s experience can tell you a lot about the appropriate treatment to address it, it’s essential to view the case from an unbiased perspective. That’s when the knowledge and experience of a medical professional spring into action.
The years you spent in medical school teaches you much about how the body functions. And because data can be crucial to the type of care the patient will receive, you must stick to the facts—and nothing but the facts. Test results and other measurable data can be useful at this stage of the process report, so remember to note them down. By doing so, it will be easier for you to distinguish symptoms from signs as you move on to the next step.
What to Avoid: This part of the SOAP note centers on quantitative data, which makes it unnecessary to elaborate statements that could’ve been done in the subjective portion of the document. The information must be specific and direct to the patient’s case, so try not to acknowledge general research statements unless you have enough data to support it.
3. Assessment: Document Impressions
With the subjective and objective elements collected, you can assess the patient’s condition and interpret it to help come up with a diagnosis. Note that some diseases are easier to identify than others due to how common their symptoms are among individuals of a particular age group or environment. But for rare and more complicated cases, you may want to spend a little more time studying the report based on its subjective and objective levels before arriving at a diagnosis. Follow-up visits may also be necessary to find out whether a patient’s symptoms persist or progress after responding to initial treatment. If the case only worsens over time, further testing will be imperative to avoid complications that could affect the patient’s overall health.
What to Avoid: There’s no need to restate what you’ve already mentioned in the first two sections of the note. Here, you need to take a step back and take one good look into the patient’s condition and see what factors contribute to their progression or regression since their first visit.
4. Plan: Determine the Course of Treatment
In this part of the SOAP note, you must create an action plan for the diagnosis. If a patient is dealing with multiple medical conditions, be sure to develop a plan for each. Addressing these concerns in your SOAP note should build a roadmap for the patient’s continuing treatment with you or under the care of other clinicians. Any instructions given to the patient regarding the kind of medications and remedies to take must reflect in the medical record as well. That way, the attending practitioner may consult the plan during the patient’s next checkup.
What to Avoid: Since you already have the patient’s case laid out for you in the treatment plan, you don’t have to repeat it in this section. Instead, you must be specific about what you want to achieve along with your plan of action to get there. You can also make adjustments to aspects of the plan that require your attention.
Ultimately, SOAP notes offer a quick and efficient way for medical practitioners to document patient encounters at the time of need. It is the responsibility of all physicians and nurses to keep these records up to date for the proper care and treatment of patients. Take note of these guidelines, and you should be able to achieve your desired goals.
