3+ SAMPLE Intake Progress Note
FREE Intake Progress Note s to Download
3+ SAMPLE Intake Progress Note
What Is an Intake Progress Note?
Benefits of Progress Notes
Elements of a Progress Note
Tips for Taking Better Nursing Notes
How to Write a Progress Note
FAQs
How do you write a better progress note?
Why is progress important for success?
How do I write a daily progress report?
What Is an Intake Progress Note?
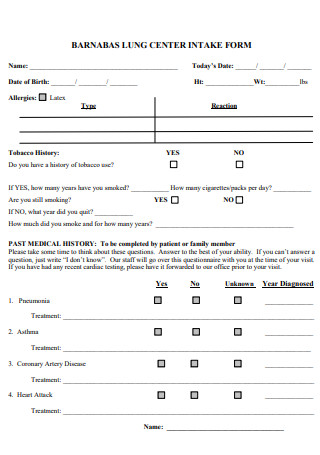
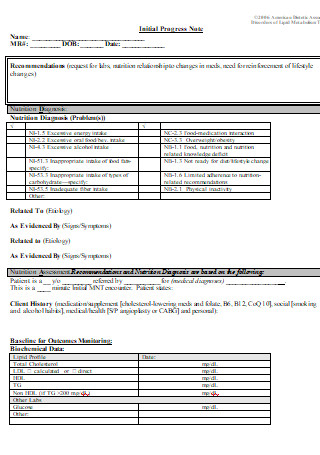
Essentially, intake progress notes list the patient’s urgent medical needs during note-taking. It could also be used by physicians, therapists, and lifestyle coordinators to monitor patients’ health, behavior, physical appearances, and movement and abilities during interactions. There are varying estimates regarding the optimal size of a patient panel and the number of patients a provider sees each day. The majority of physicians see between 11 and 20 patients every day, according to a 2018 poll. 1.3% of physicians saw between 51 and 60 patients per day.
Benefits of Progress Notes
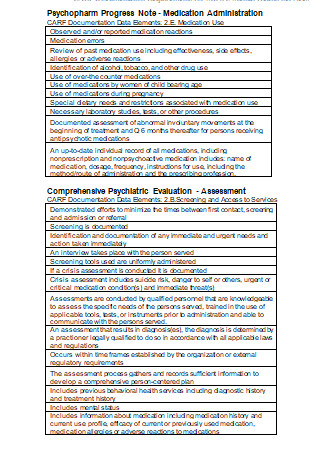
There are many reasons to keep track of progress; the following are just a few. Progress notes constitute an agreement between the client and clinician. They are where treatment objectives and plans can be discussed and decided upon before being written down to track treatment progress. Notes on progress facilitate communication within and between care teams. They allow healthcare professionals who provide care for the same client to know what transpired in the previous session or acute episode, allowing them to provide the most appropriate and accurate treatment for the presenting issue. Regardless of how good your memory is, as a healthcare professional, remembering the details of each session can place a significant mental strain on you. Writing them down provides a valuable reference point and ensures you can establish rapport with each client by recalling pertinent details about each session. Lastly, progress notes are legal documents, and you must maintain a record of each client’s care history for regulatory, insurance, and lawful purposes.
Elements of a Progress Note
If you have spent time in a therapy clinic, you will understand the significance of a detailed case report. Progress notes are imperative for correct memory, therapeutic monitoring, and effective teamwork. In addition, they are essential for insurance reimbursement. For any progress note to be successful and relevant for insurance purposes, we recommend including the following ten elements:
Tips for Taking Better Nursing Notes
Much information must go back and forth between patients, doctors, and nurses in the medical field. Most of the time, nurses take notes that are put into the patient’s file and can be looked at by anyone who might need them. With the help of the following tips, nurse practitioners can write accurate, consistent notes that make it much easier to get good patient results.
1. Standardized forms for note-taking save time and effort.
It is advantageous to write notes using the same format to make note-taking more consistent and expedite exporting the information from into medical records. Having a standard outline or form for recording important notes or highlights from interactions with patients and medical staff eliminates the need for nurses to sort through messages before using them. When digital charting systems are unavailable, it is essential to be precise and use utterly legible handwriting. Medical records are typically legal documents, so when corrections to notes or records are necessary due to an error, they must always be approved by a nurse administrator.
2. Notes should be taken quickly; do not delay
Due to the fast-paced nature of medical facilities, nurses should constantly take notes as soon as possible. If note-taking is delayed for too long, other events with higher importance may occur, preventing nurses from collecting vital information. As time passes and new situations develop, nurses may need help capturing important patient information. This could be dangerous, as failure to communicate critical information could result in negative consequences for the patient.
3. Avert your eyes from slang, jargon, and acronyms.
Using abbreviations can render a nurse’s notes invalid, as other medical professionals may not recognize the language. Assuming that all colleagues understand uncommon professional jargon could be problematic, as the medical professional reading it may need to comprehend the nurse’s intended message. If an important message is misunderstood, there is a risk of administering improper treatment to a patient.
4. Only record facts and significant occurrences
The most excellent method to guarantee that medical records are accurate and helpful is to include only factual, first-hand information when composing notes. Even when numerous events co-occur, nurses must focus on making notes in chronological sequence as they occur. When taking notes, nurses should always observe confidentiality while maintaining consistency. Patients and their caretakers may request access to their medical records; therefore, it is essential to be utterly truthful while avoiding disclosing confidential information when taking medical record notes.
5. Document all pertinent observations and details
Important information that cannot be classified as an “event” should also be recorded based on the nurse’s assessment of what is essential to the patient’s care. In many instances, keeping regular records of vital biological measurements such as visual acuity, blood pressure, pulse, temperature, and respiration diagnostics can be advantageous. This is best accomplished using the data presented in charts and then filing the charts into the patient’s discharge notes. Writing about what will occur after the patient is discharged and recording plans for future treatment can also be beneficial. These notes may include information on the medications that will be prescribed, as well as methods to schedule a follow-up appointment with the patient to assess their ability to adhere to defined plans.
6. Date and sign all documents
To maintain an organized and consistent recordkeeping system, nurses should also include the date of each note and their signature so that other medical personnel can verify that the notes were not forged. Also, patient signatures should be double-checked on consent forms and other essential data. Taking notes is not a glamorous nursing skill, but it is of the utmost importance. Understanding what to capture, when to write particular data, the right approach to organize notes, and how to communicate vital medical information will enhance a nurse’s capacity to deliver value to patients.
How to Write a Progress Note
Many medical professionals write nursing progress notes using the SOAPI method. SOAPI is an acronym for subjective, objective, assessment, and plan. Here is a list of steps for writing a nursing progress note using the SOAPI method.
1. Gather subjective evidence
After recording the date, time, and your and the patient’s names, you should begin your nursing progress note by asking the patient for information. This information is presumably subjective and confined to the knowledge and perspective of the patient. The patient’s discomfort level, the reason for their visit, and their worries are examples of subjective evidence. Consider asking family members or close friends accompanying your patient if they have seen any changes in their health. Try to act with empathy and utilize your active listening abilities to take note of your patient’s issues and demonstrate your commitment to their care.
2. Document objective details
After speaking with and listening to the patient, collect objective data to include in the progress note. This consists of the patient’s vital signs, observable symptoms, and the results of any bloodwork tests you or the physician ordered. Often, objective information supports the personal information provided by the patient, provides context for the patient’s concerns, and leads to a diagnosis.
3. Record your assessment
In this section, record patient condition notes based on the conclusions you and the patient’s primary care physician draw from the patient’s symptoms and objective data. Your evaluation also includes any medications prescribed by the doctor and the patient’s response to those medications. Attempt to observe changes in the patient’s appearance, attitude, and symptoms since admission.
4. Detail a care plan
The care plan section of your nursing progress note includes any measures you and the physician intend to take for the patient’s benefit. For instance, if the patient is scheduled to undergo an MRI, you could mention it in the progress note. Additionally, it is essential to include any pertinent information regarding the patient’s response to the care plan. For instance, if the patient declines your and the doctor’s recommendation that they return for a follow-up appointment, indicate this in the progress note.
5. Include your interventions
Your nursing progress note’s interventions section may contain a variety of information. This progress note section should primarily collect additional information regarding the patient’s care during your shift. Please include information about the times you administered medication to the patient, any requests they made, and any additional observations you have about the patient.
FAQs
How do you write a better progress note?
Ensure your notes always include the time, date, and duration of your sessions and your signature. Refer to your previous entries in the progress log for continuity. As soon as possible after each session, record your notes so you remember vital information.
Why is progress important for success?
Growth and progress allow you to achieve your objective, and in doing so, you prepare for your following purpose. When you concentrate on the goal, it can appear distant. It would help if you made the necessary effort between where you are now and the desired outcome.
How do I write a daily progress report?
Create an end-of-day (EOD) report that highlights the day’s achievements and difficulties. Include completed tasks and the amount of time consumed on each job. Identify critical accomplishments and describe any obstacles encountered. Include a daily action plan and any pertinent comments for your manager to review.
Always remember that a progress note contains confidential client information. No one besides authorized personnel should read it. Keep the notes in a safe place. If the note is stored on a computer, only authorized personnel can access it. Download our sample templates for intake progress notes if you need a template with a specific format. You are free to download any templates you desire.