50+ SAMPLE Provider Agreement
-
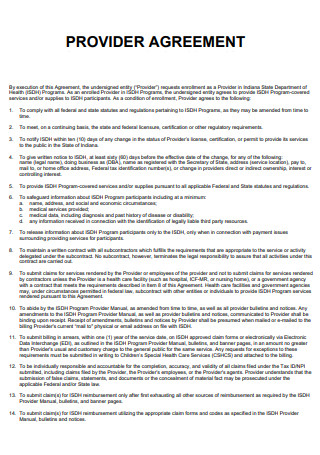
Provider Agreement
download now -

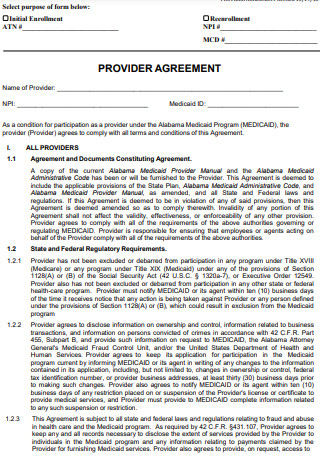
Medicaid Program Provider Agreement
download now -
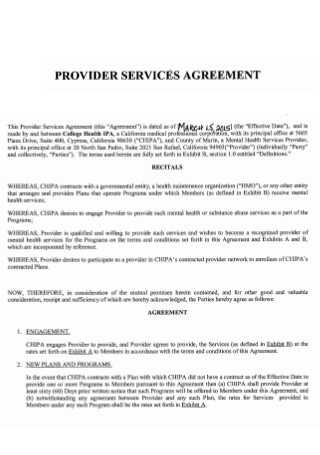
Provider Service Agreement
download now -
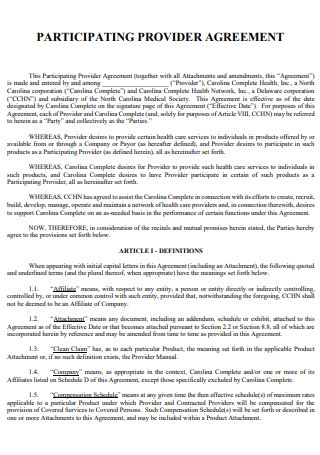
Participating Provider Agreement
download now -

Vaccination Program Provider Agreement
download now -
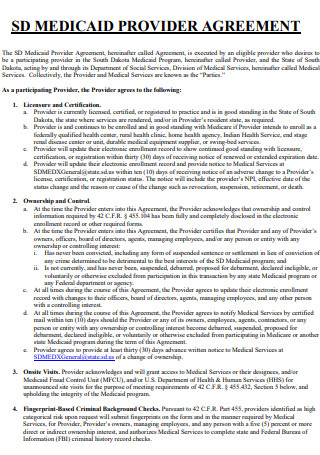
Medicaid Provider Agreement
download now -
Medical Assistance Provider Agreement
download now -
Core Provider Agreement
download now -
Allied and Ancillary Provider Agreement
download now -
Early Education Provider Agreement
download now -
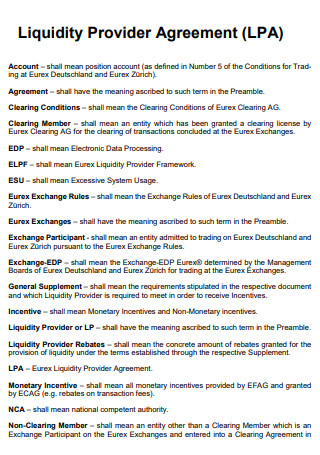
Liquidity Provider Agreement
download now -

Online Claiming Provider Agreement
download now -
Provider Agreement Enrollment Application
download now -
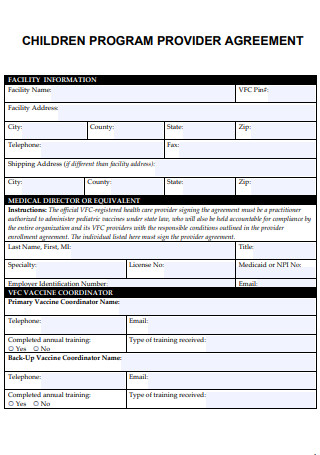
Children Program Provider Agreement
download now -
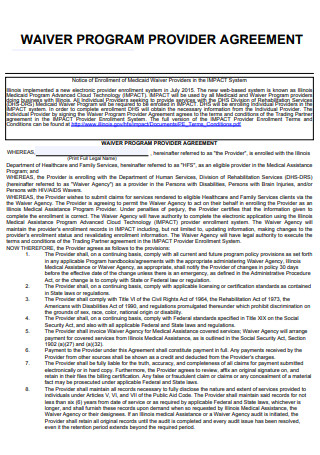
Waiver Program Provider Agreement
download now -
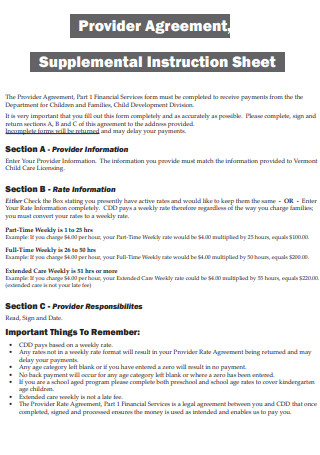
Provider Agreement Supplemental Instruction Sheet
download now -
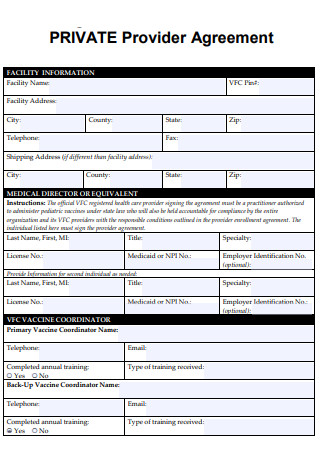
Private Provider Agreement
download now -
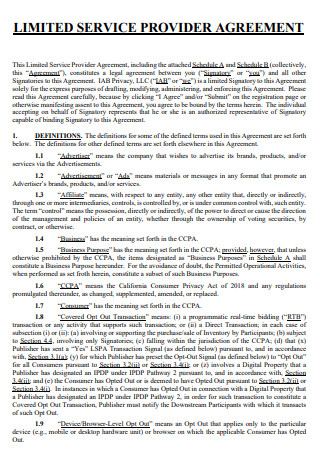
Limited Service Provider Agreement
download now -
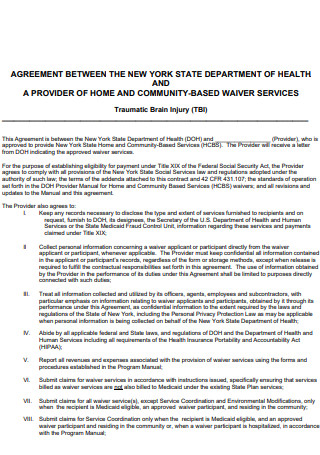
Home and Community Based Provider Agreement
download now -
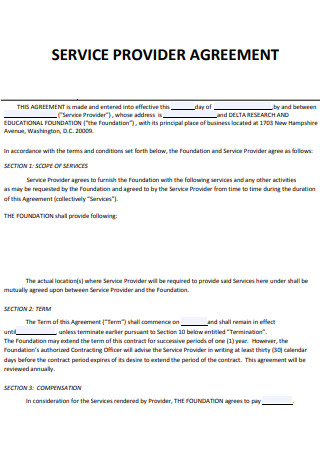
Service Provider Agreement
download now -

Provider Agreement for Qualified Hospital
download now -
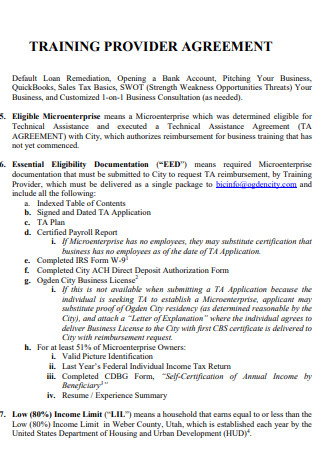
Training Provider Agreement
download now -

Individual Service Provider Agreement
download now -
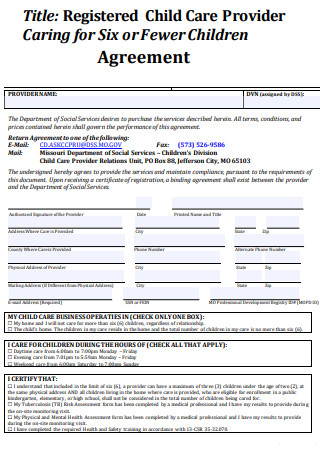
Registered Child Care Provider Agreement
download now -
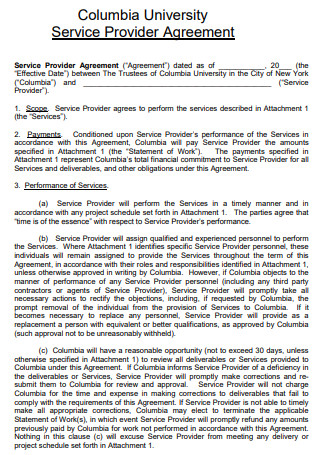
University Provider Agreement
download now -
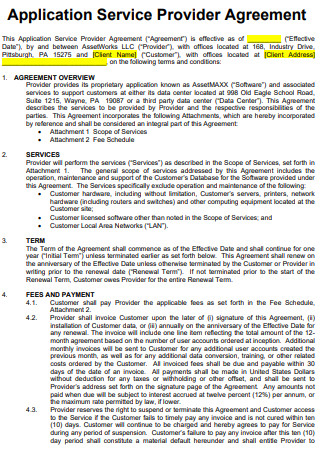
Application Service Provider Agreement
download now -
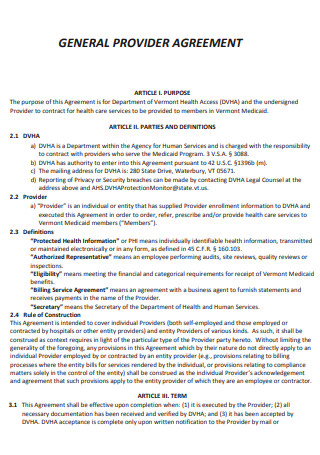
General Provider Agreement
download now -
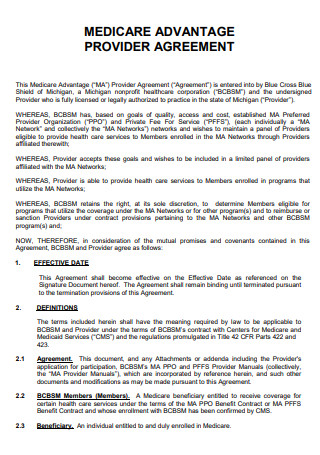
Medicare Advantage Provider Agreement
download now -

Plan Service Provider Agreement
download now -
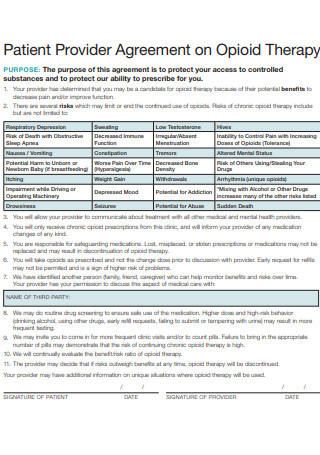
Patient Provider Agreement
download now -

Sample Provider Agreement
download now -
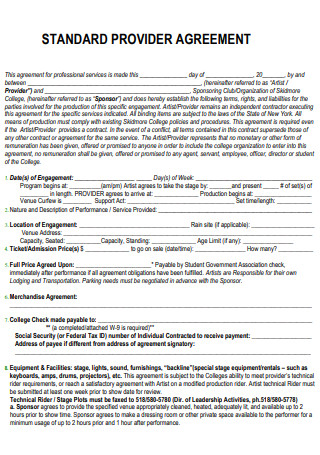
Standard Provider Agreement
download now -
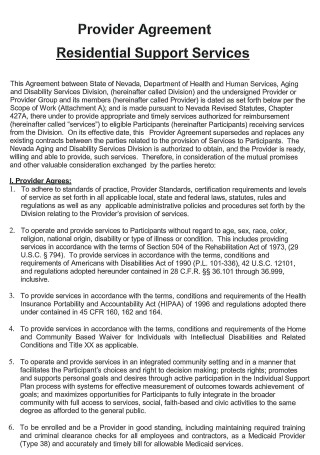
Residential Support Provider Agreement
download now -

New Provider Agreement
download now -
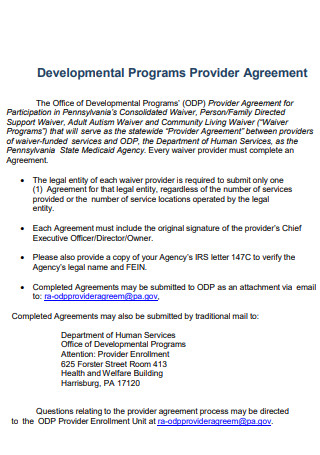
Developmental Programs Provider Agreement
download now -
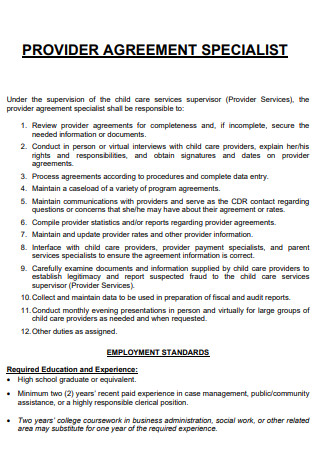
Provider Agreement Specialist
download now -
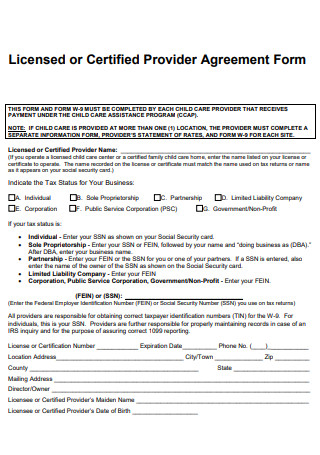
Licensed or Certified Provider Agreement
download now -
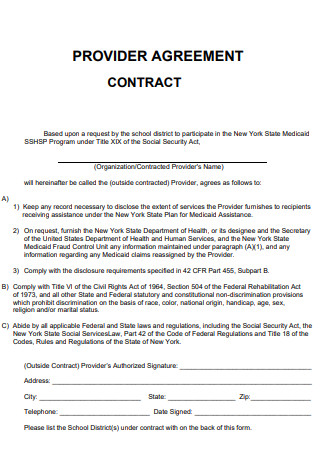
Contract Provider Agreement
download now -
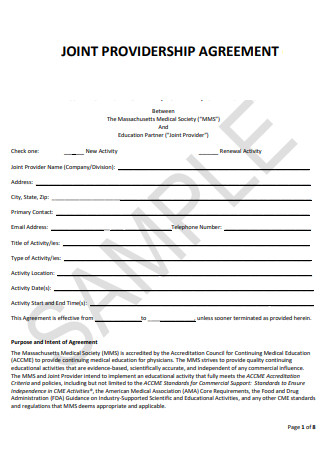
Joint Providership Agreement
download now -
Simple Provider Agreement
download now -
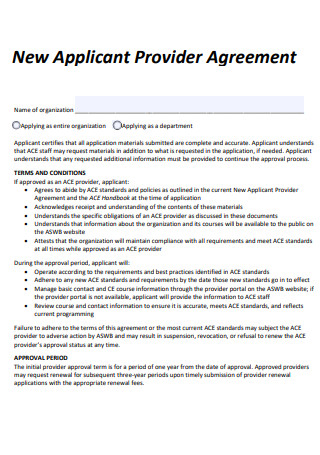
New Applicant Provider Agreement
download now -
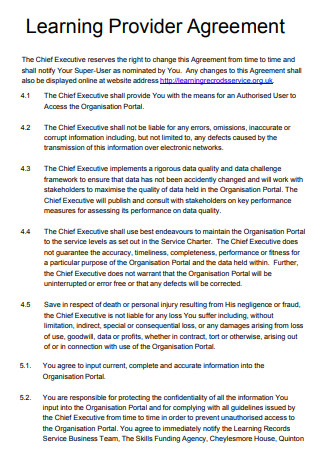
Learning Provider Agreement
download now -
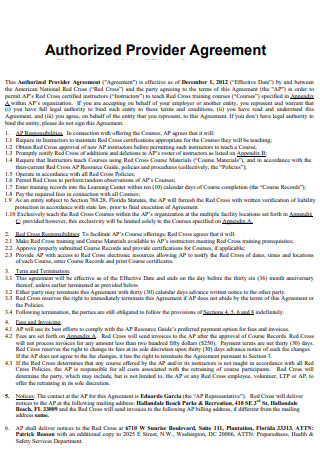
Authorized Provider Agreement
download now -

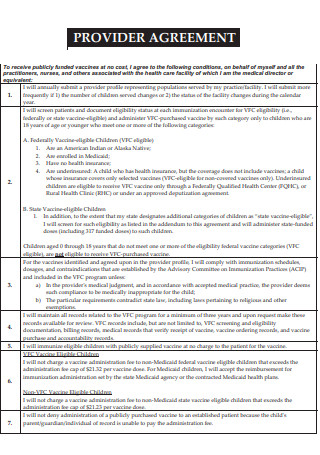
Provider Agreement to Receive State-Supplied Vaccine
download now -

Data Provider Agreement
download now -
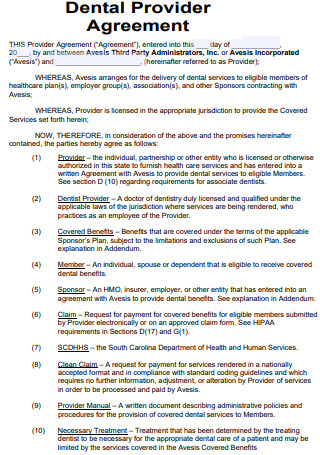
Dental Provider Agreement
download now -
Provider Site Usage Agreement
download now -
Accredited Training Provider Agreement
download now -
Provider Security Agreement
download now -
Pharmacy Provider Agreement
download now -
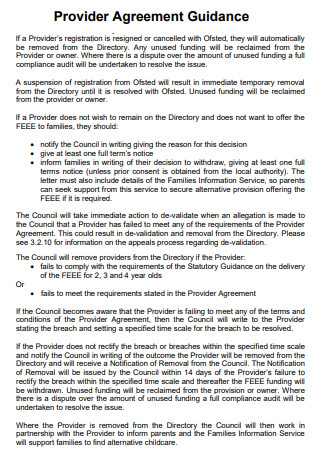
Provider Agreement Guidance
download now
FREE Provider Agreement s to Download
50+ SAMPLE Provider Agreement
What Is a Provider Agreement?
What Is Included in a Provider Agreement?
Why Do You Need to Understand Provider Agreement?
What to Watch Out for in a Provider Contract?
How to Negotiate for Better Terms in a Provider Contract?
How Do You Create a Services Agreement?
FAQs
What Is A Provider Contract Going To Do For Me?
What Is My Responsibility for Ensuring Clean Claims?
How Can I Dispute Denied Claims?
Can the Contract Be Changed?
For instance, an accountant must give his client the exact estimate of his fees. He must also inform the client that there is a chance his fees could change and that other professionals will work on the file, which could increase the total cost of the service.
What Is a Provider Agreement?
A provider agreement is a document that represents the business relationship between a provider and a payor. A provider can be either an individual physician or a healthcare facility with multiple doctors on staff. The provider administers medical services to patients. The payor is typically insurance companies, but can be individuals who are paying out of pocket for medical services. Payors pay for all (or at least some) of the cost of the patients’ medical services. The provider agreement is a vital element for any health care provider who wishes to operate a smoothly run facility with high patient satisfaction and on-time payments. However, there are many different types of healthcare provider contracts. Each are filled with lots of unfamiliar legal jargon and confusing clauses, amendments, and stipulations. In addition, to get a better idea of what to expect in a provider contract, and how to negotiate the most beneficial terms, follow along as we break down everything you need to know. By the end of this article, you will also learn the benefits of using a healthcare contract management system for your healthcare facility.
What Is Included in a Provider Agreement?
No matter how customized a provider agreement is, it typically includes standard information:
Services
Explains the general nature of the services and often includes an attached schedule that discusses the scope of the work and the deliverables involved.
Compensation
States the total amount or the periodic amount that the client agrees to pay the service provider in exchange for the work and may include an attached schedule.
Term
Lists the start and end date or the number of days, weeks, or months the contract is in effect.
Ownership
Clarifies whether the client or the service provider can claim ownership over any physical products or intellectual property produced during the project.
Relationship
States that the service provider remains an independent contractor who is not employed by the client.
Liability
Confirms whether the client or the service provider has limited liability for any aspects of the project.
Insurance
Lists the type of insurance coverage the service provider must have, such as workers’ compensation, commercial general liability, professional liability, or property insurance.
Change in the Work
Specifies whether either party can change the scope of work and what procedure they must follow to do so.
Confidentiality Clause
States whether either party must keep the project confidential.
Non-compete Clause
Clarifies whether the service provider can work with one of the client’s competitors.
Non-solicitation Clause
Specifies whether the service provider is prohibited from soliciting the client’s customers or peers.
Assignment
Clarifies whether the service provider may subcontract the project.
Termination
Explains how many days’ notices either party must provide before ending the agreement.
Why Do You Need to Understand Provider Agreement?
To receive reimbursement for medical services, providers depend on provider contracts in healthcare. The agreement details all of the information that needs to be collected by physicians from their patients before sending a claim for reimbursement to the payor. Reimbursement can be delayed or even denied if the claim procedures don’t strictly follow the guidelines set up in the provider contract.
To ensure correct claim procedures and a steady revenue flow, here are a few essential details that will be outlined in any provider agreement:
- Rates for billed medical services
- Time frame within which the health care provider must submit a claim for reimbursement
- Time frame within which the payor must reimburse the provider once a claim is received
- Scope and type of health care services that are covered by the payor
- Procedure by which the provider can dispute a claim denial
- How many days either party must notify the other before terminating the contract
Before signing a provider agreement, it is important to understand what the contract means for you or your business. Keep these standard legal considerations in mind:
Liability
A services agreement can limit liability for either party, but terms should be reasonable to stand up in court.
Obligations
Clients must agree to work with the service provider by sharing required information and providing equipment or venue access.
Rate Changes
Both parties should agree whether or not the service provider may change the rate and how much notice they will provide.
Termination
Either party should be able to end the contract with a written notice, and the agreement should end automatically if either party violates the terms.
What to Watch Out for in a Provider Contract?
There will always be terms or conditions to look out for in a provider agreement. Although these parts of the contract may seem minor, taking up only a few words, they can still have a major impact on your business. Here is a few final things to watch out for:
With any agreement, you should consider the common challenges in provider contract management and take a deeper dive into each challenge.
How to Negotiate for Better Terms in a Provider Contract?
The first step in any successful provider contract negotiation occurs long before you reach out to the payor with demands. Prior to engaging in formal negotiations, you should arm yourself with as much knowledge as possible. Familiarize yourself with your current contract, and research the legalese to become more comfortable speaking the payor’s language. Then, engage in each of the following best practices:
Gather Internal Data
Once you have mastery over the contract’s components, it is time to gather internal data. Because most providers are contracted with multiple payors, start by reviewing your top 5 or top 10 payors. Determine your most frequently billed services and compare the payment amounts you receive from each of your top payors. With this data, you can analyze the financial performance of each provider contract. Then, you can set target goals for the negotiation.
You can also analyze your past claims to find out which payors reimburse you the least for certain health care services. With that data, you can argue in future negotiations that the payor should offer a reimbursement rate that is more in line with the rest of the marketplace.
Survey Patient Satisfaction
Another important data point to collect is the rate and quality of patient satisfaction. Because this data has some subjective elements, you may need to rely on patient surveys. Still, positive patient surveys can demonstrate your facility’s efficiency and effectiveness.
You can also survey other physicians who refer patients to your facility, as well as any hospital administrators you work with. Systematically surveying the people in your business landscape can provide a clear picture of your value.
Conduct Market Research
Think about your facility in the context of your surrounding area. Find out information on these key questions:
- Is there a niche service that your facility specializes in?
- How many other facilities in your area offer the same services as you?
- Do you have a good reputation among top referring physicians in your area?
- How does your facility compare in size to those around you?
- For how many residents are you the closest medical facility?
Suppose you can demonstrate that your facility is an integral part of your community, a unique healthcare offering, and a top option for patients. In that case, you will have more leverage in contract negotiations.
Prepare Specific Demands
When you finally sit down to engage in proper negotiations with your payor’s representatives, you should have ample data to back up your demands. Keep in mind that your demands should be specific and evidence-based. It’s much easier for the payor to deny a general plea for better contract terms than, for example, a data-supported demand for a 5% increase to your ultrasound therapy reimbursement rate.
How Do You Create a Services Agreement?
To develop a services agreement, here are the steps to follow:
Step 1: State the Service Provider and Client
Take care to list the legal names and include the mailing addresses for all parties involved.
Step 2: List the Services Included
In the main body of the agreement, state the nature of the services concisely. In an attached schedule, describe the scope of the work and mention any deliverables.
Step 3: State the Compensation Amount and Outline the Schedule
Along with the payment amount, include payment dates or frequencies.
Step 4: Clarify Which Party Retains Ownership
Whether the services include physical goods or intellectual property, state whether the service provider or the client assumes ownership.
Step 5: Include Any Confidentiality or Competition Terms
If the client requires the service provider to refrain from discussing the project or working with competitors, state any guidelines the provider must follow.
Step 6: List Any Applicable Indemnity or Liability Limitations
Include any insurance requirements.
Step 7: Execute the Agreement
Once both parties agree to the terms and sign the contract, the provider agreement becomes legally binding.
FAQs
What Is A Provider Contract Going To Do For Me?
Before signing, you should do some accounting and assemble hard data that proves the provider contract will lead to a positive financial outcome for your healthcare facility. Payors do not necessarily have your best interest in mind.
What Is My Responsibility for Ensuring Clean Claims?
A clean claim is one that does not require any additional information in order to be processed and approved for reimbursement. Ideally, all of your claims will be clean, and you will always receive reimbursement on time. The provider contract will stipulate exactly what information needs to be included with every claim. Make sure you know what you need to do.
How Can I Dispute Denied Claims?
Payors sometimes deny reimbursement to providers for services rendered. Often, providers feel they are entitled to that reimbursement and seek to reverse the denial decision. In some cases, you may have to rely on formal litigation to arbitrate your dispute. Be wary of contract language that forbids you from seeking legal recourse to claim disputes. Know what your options are for recouping.
Can the Contract Be Changed?
Some provider contracts contain what is called unilateral amendment language. If your provider contract allows for unilateral amendments, it means the payor can alter the contract without your permission. In many unilateral amendment cases, the payor may not even need to notify the provider that changes have been made to the contract. Avoid this if possible.
Providers are in the business of keeping their patients healthy. But confusing payer contracts riddled with “legalese” and other complicated provisions can get in the way of improving patient outcomes. Moreover, provider contracts define and explain a provider’s reimbursement arrangement for delivering healthcare services to patients covered by a specific health plan. The contracts cover everything from reimbursement rates and provider networks to medical necessity and provider credentialing. Understanding complex provider contracts are key to ensuring timely, correct reimbursement and keeping a practice’s doors open. Knowing the ins-and-outs of each contract is also crucial to avoiding claim denials, drawing patients to the practice, and offering comprehensive and reimbursable services to patients.
Despite the importance of provider contract knowledge, providers, and even their practice administrators and revenue cycle leaders, may feel less than confident when up against payer organizations with legal departments, financial analysts, and advanced software systems. The entire process of contracting and renegotiating with payers is complex, which could make providers feel like they have the disadvantage.
