18+ SAMPLE Clinical Development Plan
-

Clinical Development Plan
download now -
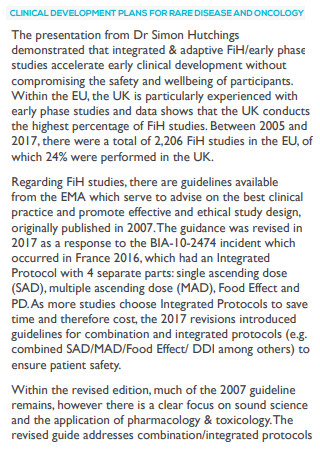
Clinical Development Plan for Rare Disease and Oncology
download now -

Clinical Trails Comprehensive Development Plan
download now -

Data Standardization Planning for Clinical Development Programs
download now -

Clinical Development Plan Guide
download now -
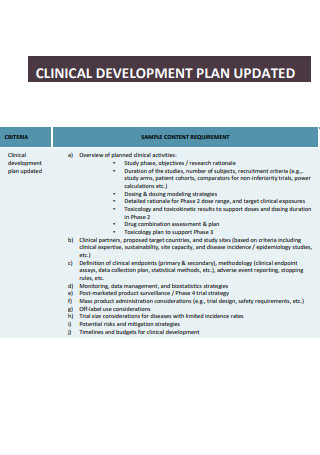
Clinical Development Plan Updated
download now -
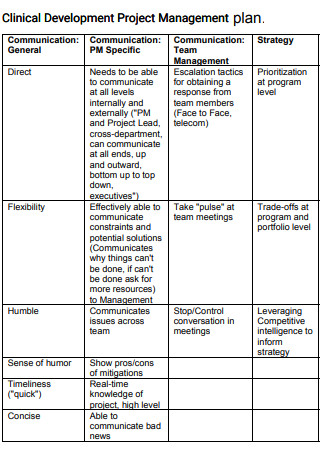
Clinical Development Project Management Plan
download now -
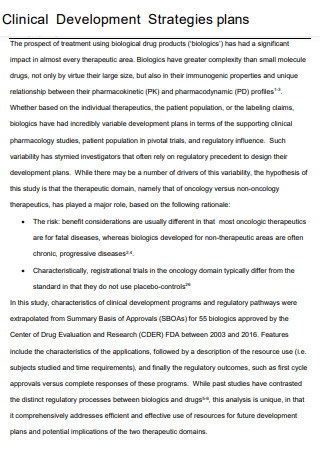
Clinical Development Strategic Plan
download now -

Sample Clinical Development Plan
download now -
Clinical Evaluation Development Plan
download now -
Robust Clinical Development Plan
download now -

Modern Clinical Development Plan
download now -
Clinical Development Planning
download now -
Adaptation in Clinical Development Plan
download now -

Precision BioSciences Clinical Development Plan
download now -

PreClinical Development Plan
download now -

Optimizing Clinical Development Plan
download now -

Technology for Your Clinical Development Plan
download now -
Simple Clinical Development Plan
download now
FREE Clinical Development Plan s to Download
18+ SAMPLE Clinical Development Plan
What Is a Clinical Development Plan?
Important Elements of a Clinical Development Plan
Types of Clinical Research
Problems That Can Be Encountered During Drug Development
Steps of Clinical/Drug Development
FAQs
Orphan Drugs can also be developed during the clinical development process. What is it?
Drug delivery methods, such as topical delivery, are analyzed in the clinical research phase of clinical development. What is a topical delivery method?
What is the role of the FDA in clinical/drug development?
What Is a Clinical Development Plan?
First of all, what is clinical development all about? Well, it is a collective term that is used to properly identify the entire process of introducing a breakthrough drug or medication device to the market. Clinical development consists of drug discovery and its subsequent development, the pre-clinical research phase which is accordingly done on microorganisms or animals, and the clinical trial phase which is done on humans. As it refers to introducing a new drug to the market, clinical development can also be called drug development.
A clinical development plan is an essential document that is needed whenever an intent to develop a new drug or medical therapy is introduced. It serves as the blueprint for a drug’s whole clinical research strategy. The clinical development plan defines the important route for the clinical program, including development evaluation and decision points, as well as project resources (such as people and money) estimations. Additionally, as more information becomes available from the results of studies, this document must also be accordingly updated and adapted.
Important Elements of a Clinical Development Plan
Listed and properly elaborated below are the main elements that have to be included in creating a clinical development plan:
Types of Clinical Research
Here are the different types of clinical research that are used by the researchers based on what they are studying:
Problems That Can Be Encountered During Drug Development
Clinical development is also known as drug development and often times it is not a very smooth process. Listed below are the various challenges that can be encountered during this process:
Steps of Clinical/Drug Development
Clinical development has become a complex process throughout the years, requiring more and more testing phases before getting approved. The process of clinical development involves a number of critical steps. all of which will be discussed accordingly below.
-
1. Discovery and Development Phase
This is the first step of the clinical development phase. This step comprises screening hits, medicinal chemistry, and hit optimization to eliminate possible drug adverse effects and thereby increase affinity and selectivity. It also entails high-throughput screening, hit-to-lead operations, and lead optimization procedures. This stage of the medication development process also improves effectiveness or potency, metabolic stability (half-life), and oral bioavailability. The process of drug discovery concludes when one lead chemical for a candidate drug is discovered, and the drug development phase begins.
-
2. Preclinical Research
After the discovery and development process, this step then follows. The preclinical research phase involves testing to establish the medicine’s effectiveness and safety. The researchers assess the drug’s potential advantages and methods of action, ideal dose and delivery route or routes, adverse effects, interactions with other medicines, and efficacy when compared to similar medications in this phase. The medicine is next tested on non-human subjects to determine its effectiveness, toxicity, and pharmacokinetics. Scientists undertake these experiments in vitro (externally) and in vivo (internally) with unlimited doses.
-
3. Clinical Development/Clinical Trials
After the preclinical research phase, this step then follows. This step usually involves the clinical trial phase to finetune the drug in order to make it suitable for human consumption or use. It should be noted that the trials need to be safe and must be completed using the given budget and also using an approved methodology to confirm that the drug works properly within its intended objective. Additionally, the clinical trial phase must be rigorous, set up correctly. and take in plenty of participants to improve the study’s effectiveness.
-
4. Review
After the clinical development/trial phase of the new drug, and once the results have been confirmed or finalized, a review then follows. A review is usually performed by a higher governing body such as the FDA. In FDA’s case, in this process, they either approve or disapprove the application that is submitted by the drug company. The timeline may be standard or fast-tracked depending on the applications and how important is it to get patented immediately. Sometimes, new medications may be approved more quickly if there is substantial evidence of a favorable impact on a surrogate goal rather than proof of an impact on the real therapeutic benefits provided by the treatment. Having a drug approved more quickly can mean that there is a possibility that it can cure more severe health conditions. Applications can also fail, however, if the performance is proven to be inadequate or if it is too toxic.
-
5. Monitoring
Once a new drug gets approved and once it has been manufactured, this step then follows, which is called the monitoring phase. The monitoring is usually done through the use of a database called the adverse event reporting system database. This database assists the regulatory agency in implementing its post-marketing safety monitoring program. Various manufacturers, health professionals, and consumers can then use this program to report concerns with licensed pharmaceuticals.
FAQs
Orphan Drugs can also be developed during the clinical development process. What is it?
An orphan drug is a pharmacological agent created to treat medical problems that would be unprofitable to produce without state funding. The disorders that orphan drugs treat are known as orphan diseases. Patients suffering from rare diseases that must be treated with orphan medications must be kept up to date on scientific and therapeutic advances and they must be entitled to the same level of treatment as any other patient. Incentives for the health and biotechnology sectors have already been created to boost research and development in the field of orphan pharmaceuticals.
Drug delivery methods, such as topical delivery, are analyzed in the clinical research phase of clinical development. What is a topical delivery method?
Topical drug delivery refers to formulations such as ointments, creams, lotions, or transdermal patches that transport a medication into the body by absorption. Topical administration is more beneficial for a patient’s skin or muscle disorders, and patients prefer it since it is non-invasive and allows them to self-administer the drug.
What is the role of the FDA in clinical/drug development?
The role of the FDA in clinical development is that they are the ones who are interpreting laws, rules, and regulations and distributing policy pronouncements that would otherwise be confusing. The FDA also directs medication development through advisory committee meetings which can be confidential or open. These meetings help the regulatory review and approval process by introducing together specialists to assess data, recommend the need for new studies, and address relevant questions formulated by the FDA to assist in resolving scientific or clinical issues related to the drug development phase or a specific product approval.
As stated earlier, a carefully planned and created clinical development plan serves as the foundation of effective clinical development, carefully lays out the entire development life cycle along with its subsequent goals, clearly states what types of documentation is needed for each of the development stages, and most of all serve as a vital paper when a company tries to develop and introduce a new form of therapy or drug to the public. When developing one, it should be noted that it needs to be adaptable as new facts emerge over the course of the clinical development process. In this article, blank templates of a clinical development plan are readily available to you so that you have a reference to use when you need to make one.
