Nursing Care Plan Samples
-
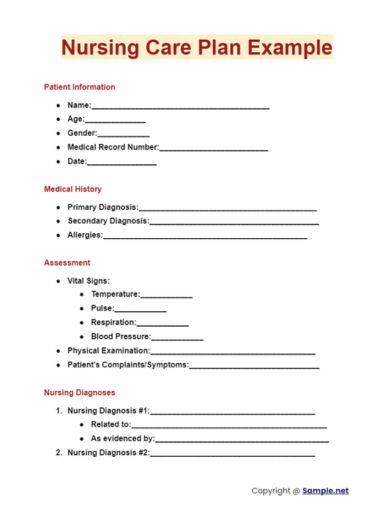
Nursing Care Plan Example
download now -
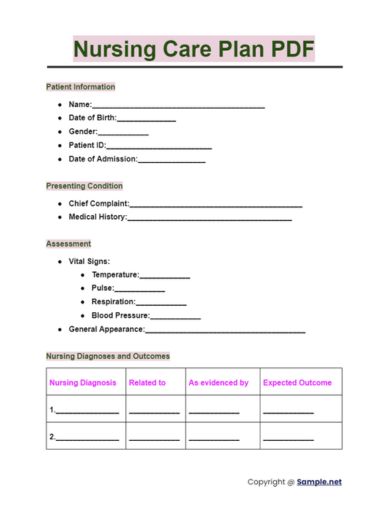
nursing-care-plan-pdf
download now -
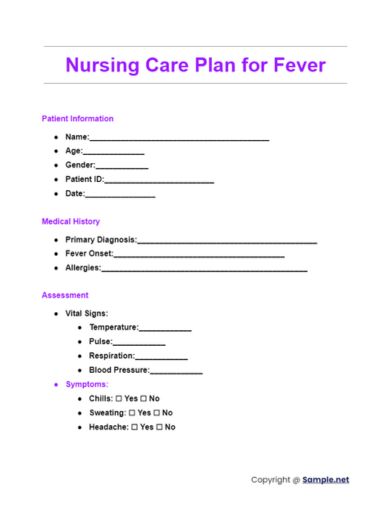
Nursing Care Plan for Fever
download now -
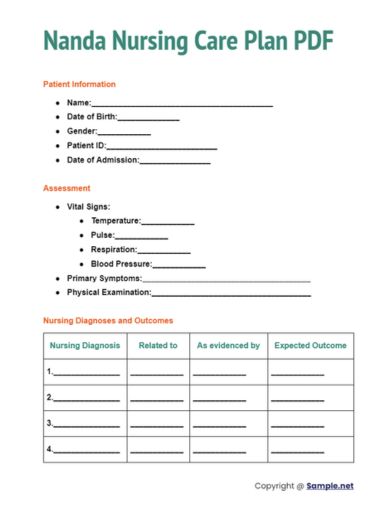
Nanda Nursing Care Plan PDF
download now -
Nursing Care Plan Template
download now -
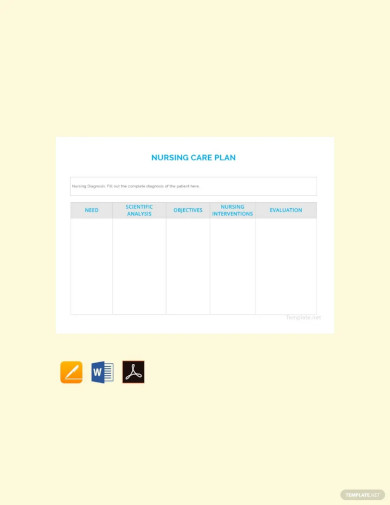
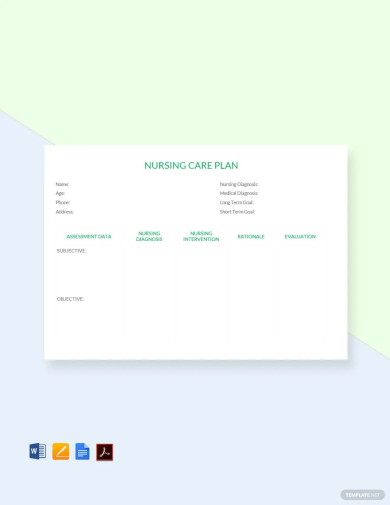
Free Blank Nursing Care Plan Template
download now -

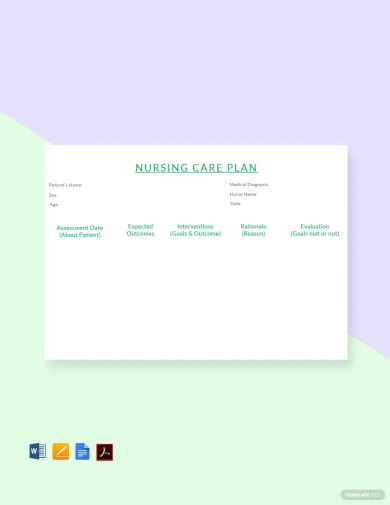
Sample Nursing Care Plan Template
download now -
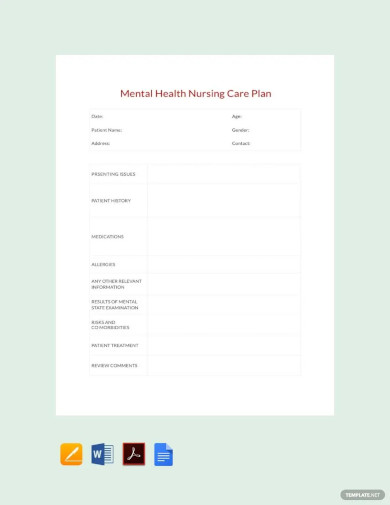
Mental Health Nursing Care Plan Template
download now -
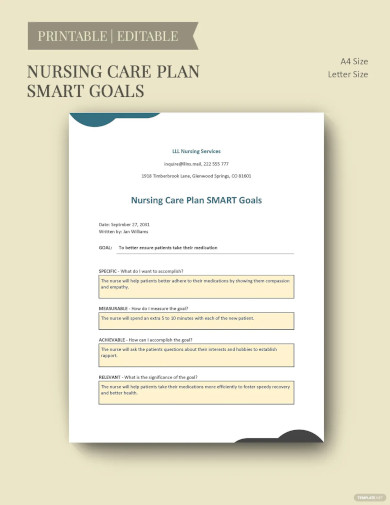
Nursing Care Plan Smart Goals Template
download now -
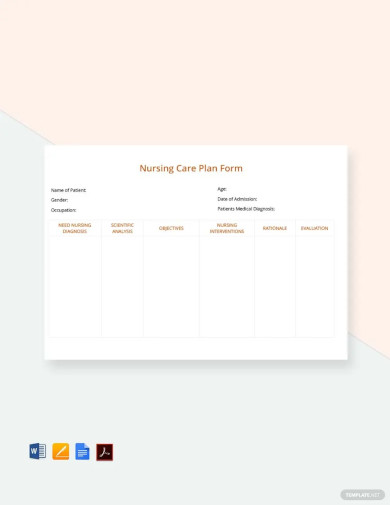
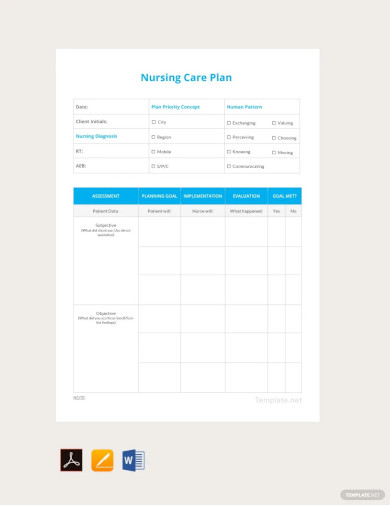
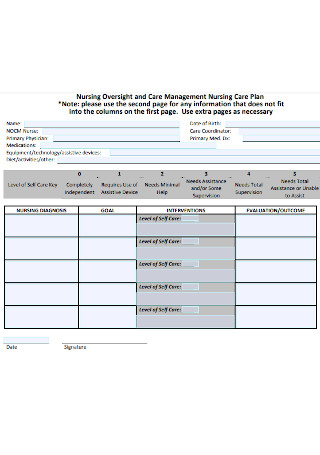
Nursing Care Plan Form Template
download now -
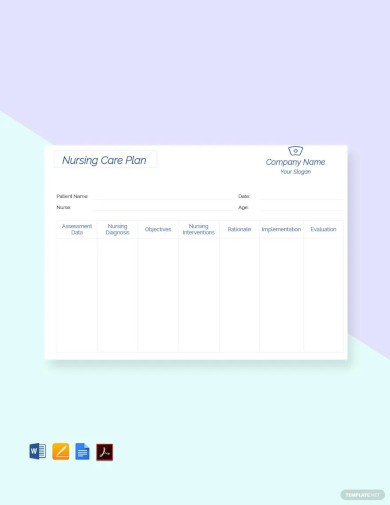
Printable Nursing care plan Template
download now -
Free Nursing Care Plan
download now -
Free Nursing Care Plan Example
download now -
Free Simple Nursing Care Plan Template
download now -
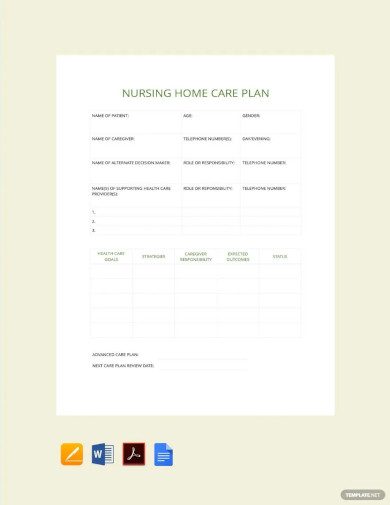
Nursing Home Care Plan Template
download now -
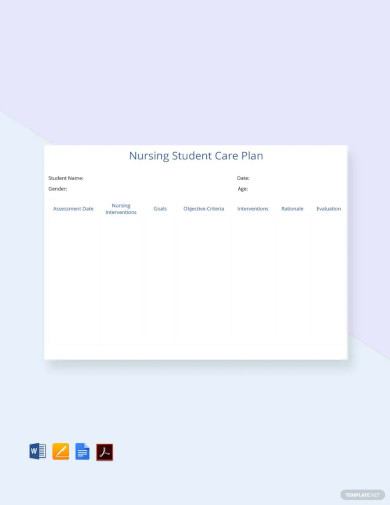
Free Nursing Student Care Plan Template
download now -

Editable Nursing Care Plan Template
download now -
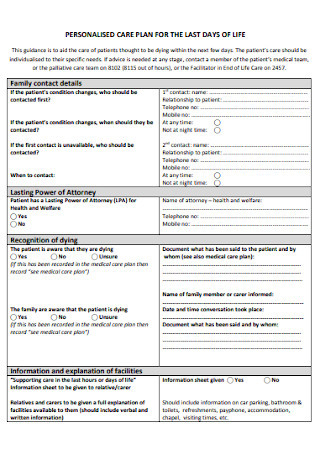
Personalized Nursing Pain Care Plan
download now -
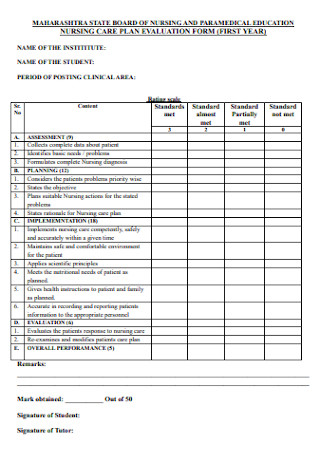
Hypertension Nursing Care Plan Evaluation Form
download now -

Nursing Fever Assessment Care Plan
download now -

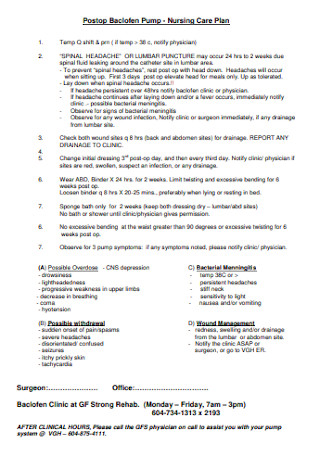
Nursing Clinic Infection Care Plan
download now -

Nursing Process Acute Pain Care Plan
download now -
Nursing Anxiety Care Plan Format
download now -
College Nursing Dehydration Care Plan
download now -

Basic Nursing Asthma Care Plan
download now -

Hospital Nursing Fracture Care Plan
download now -
School of Nursing Pneumonia Care Plan
download now -

Nursing Performance Abdominal pain Care Plan
download now -

Nursing Hyperthermia Diagnoses Care Plan
download now -

College Nursing Anemia Care Plan
download now -

Simple Nursing Diagnosis Care Plan
download now -

University Hospital Nursing Depression Care Plan
download now -

Proposal of Nursing Headache Care Plan
download now -
Development of Nursing Constipation Care Plan
download now -
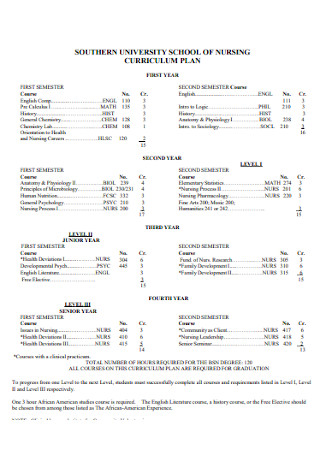
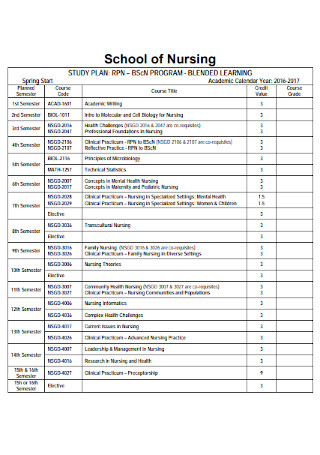
Nursing Labor Care Curriculum Plan
download now -
Nursing Business Knowledge Deficit Care Plan
download now -
Nursing Study Malaria Care Plan
download now -

Simple Nursing Quality Wound Care Plan
download now -

Diarrhea Nursing Care Plan
download now -

Urinary Tract Infection Nursing Care Plan
download now -
Nursing Program Dengue Care Plan
download now -
Nursing Management Heart Failure Care Plan
download now -

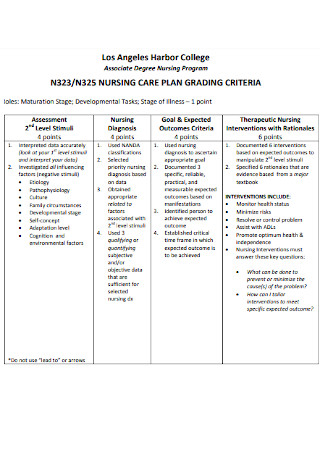
Formal Nursing Care Plan
download now -

Nursing Care Plan of Child with Diabetes
download now -
Printable Nursing Care Plan
download now -
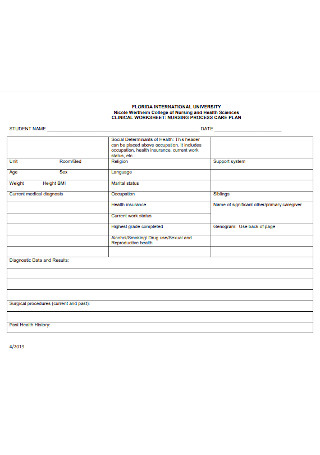
Nursing Care Plan Worksheet
download now -

Nursing Patient Care Plan
download now -
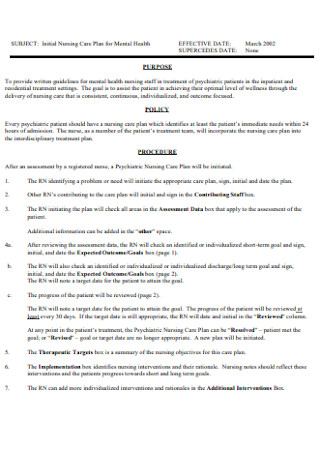
Nursing Care Plan for Mental Health
download now -

Plan of Nursing Care
download now
FREE Nursing Care Plan s to Download
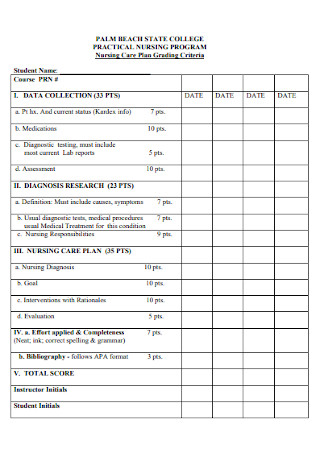
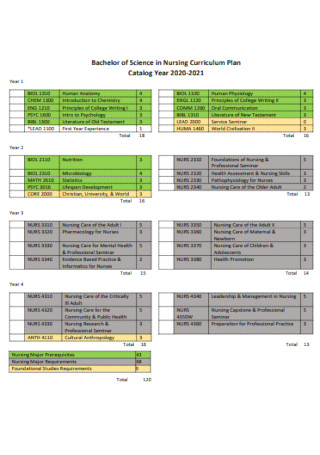
Nursing Care Plan Format
Nursing Care Plan Samples
What is Nursing Care Plan?
What Is a Performance Improvement Plan?
How to Create a Nursing Care Plan
Importance of Nurse Care Plans
Different types of Care Plans
Is there a specific care plan format to follow?
What are other considerations in writing a care plan?
Are nursing interventions the same as physician interventions?
Can nurses question the physician’s intervention orders?
What are some examples of nursing care plans?
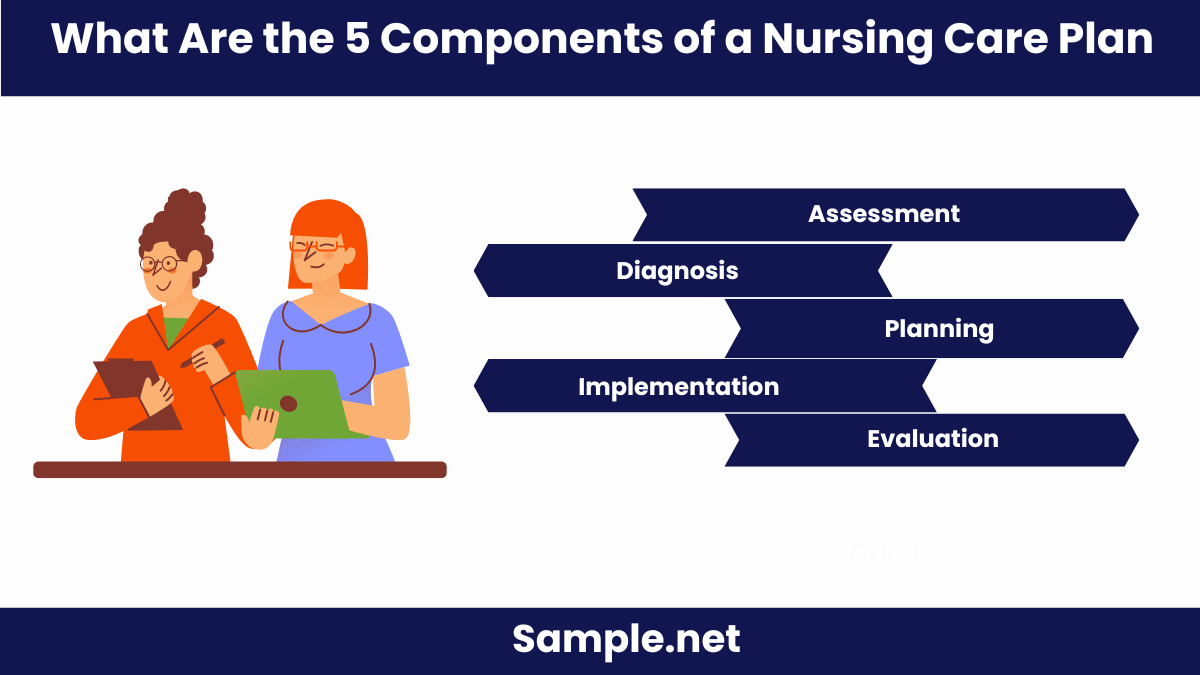
What Are the 5 Components of a Nursing Care Plan?
How Do You Write a Nursing Care Plan?
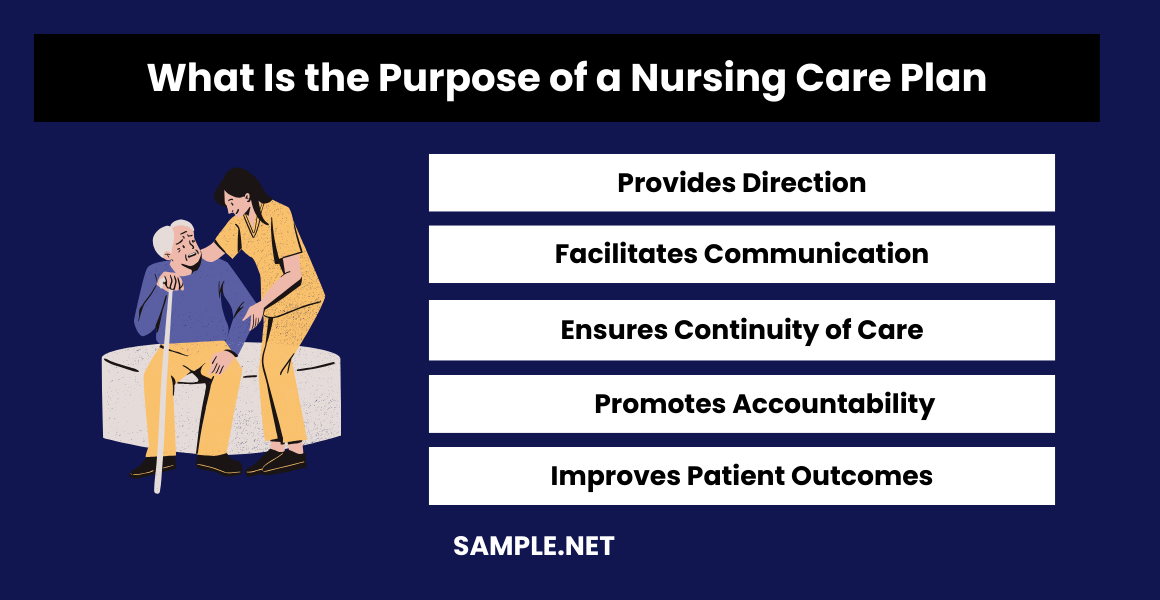
What Is the Purpose of a Nursing Care Plan?
What Is Included in a Nursing Plan?
What Are the 5 Steps of the Nursing Care Plan?
How to Develop a Care Plan?
What Are the Two Types of Nursing Care Plan?
What Is a Patient’s Care Plan?
What Is the Priority of a Nursing Care Plan?
How to Show Compassion as a Nurse?
What Are the Nursing Notes in a Care Plan?
How to Develop a Care Plan?
Download Nursing Care Plan Bundle
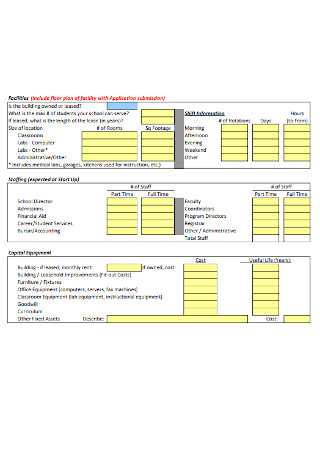
Nursing Care Plan Format
Patient Information
- Name:
- Age:
- Gender:
- Medical Record Number:
- Date:
Medical History
- Primary Diagnosis:
- Secondary Diagnosis:
- Allergies:
Assessment
- Vital Signs:
- Temperature:
- Pulse:
- Respiration:
- Blood Pressure:
- Physical Examination:
- Patient’s Complaints/Symptoms:
Nursing Diagnoses
- Nursing Diagnosis #1:
- Related to:
- As evidenced by:
- Nursing Diagnosis #2:
- Related to:
- As evidenced by:
Goals and Expected Outcomes
- Short-term Goals:
- Goal #1
- Goal #2
- Long-term Goals:
- Goal #1
- Goal #2
Nursing Interventions
- Intervention #1:
- Rationale:
- Frequency:
- Intervention #2:
- Rationale:
- Frequency:
Evaluation
- Goal #1 Met/Not Met:
- Evidence:
- Goal #2 Met/Not Met:
- Evidence:
What is Nursing Care Plan?
A Nursing Care Plan is a formal document that outlines the nursing care to be provided to a patient. It includes detailed assessments, diagnoses, interventions, and evaluations to ensure comprehensive and individualized care. Nursing Care Plans help nurses to systematically plan and deliver patient care, ensuring that all patient needs are met effectively. These plans are essential tools in nursing practice, aiding in communication among healthcare team members and improving patient outcomes.
What Is a Performance Improvement Plan?
A nursing care plan is a formal document that includes all of the patient’s health information and identifying their current needs and anticipating the potential risks. It is a means among nurses to communicate with fellow nurses, patients, and other healthcare providers to achieve care outcomes. It also ensures that the quality and consistency of care in patients remains.
Having a nursing care plan will ensure that everyone involved in patient care is on the same page, thus minimizing errors. It’s a document that healthcare providers use as a reference since all patient information is on it such as diagnoses, goals of treatment, and specific nursing orders (like what needs to be observed or actions to perform) as well as plans for evaluation. As a patient’s condition improves or changes, the information on the care plan is also updated with the new information as it presents itself. You should also take a look at our Nursing Incident Report
Depending on the workplace, nursing care plans may vary. But in most cases, it includes all the elements and contains the same information such as the diagnoses, goals or anticipated outcomes, nursing orders, and evaluation.
How to Create a Nursing Care Plan
The best nursing care plan requires a step-by-step approach and goes beyond the nursing diagnosis list. In creating a care plan, it must have all relevant information about the patient. Apart from knowing and understanding patient conditions, diagnoses, and their definitions, healthcare providers are required to have critical thinking. Follow these steps to develop a care plan for your patient.
Step 1: Data Collection and Assessment
The first step in nursing care plan creation is the data collection and assessment. To begin, one should ask what type of data is collected to identify the patient’s current medical condition and health problems. The American Nursing Association (ANA) states that the assessment process must include different factors such as physical, psychological, sociocultural, spiritual, economic data, and lifestyle. The most common approach to this is through an interview and physical examinations. You should also take a look at our Audit Plan
It’s also important that nurses review the patient’s medical history, diagnosis, and lab test results, as well as medications for any diseases or mental health issues. Through this step, nurses can identify the risk factors and pertinent information which is critical so that they can make a diagnosis. You should also take a look at our Care Plan
Step 2: Data Analyses and Diagnoses
After collecting patient data and assessment has been done, a diagnosis has to be made. A good care plan should define a diagnosis after analyzing and taking into consideration all gathered information about the patient. Usually, analysis of data involves comparison of patient data versus standards, clustering of cues, and identifying gaps and inconsistencies. You should also take a look at our Cleaning Service Business Plan
One of the most cited references is the NANDA-I nursing care plan diagnoses as a way to identify, focus and deal with specific patient needs and how to respond to actual high-risk health problems. Having a uniform standard of diagnoses eliminates confusion moving forward in the treatment and care plan of the patient. You should also take a look at our School Improvement Plan
Step 3: Data Collection and Assessment
Once diagnoses have been made, prioritization of findings should be established to determine the sequence of treatment and procedure to address patient needs. In this step, proper diagnoses are ranked based on their impact on patient health–life-threatening health problems are given high priority, and others determined to be either medium or low-risk are dealt with after. The patient’s values, beliefs, their own priorities, as well as the availability of resources, and urgency of other factors must also be considered during prioritization. For example, if a diabetic patient recently had a stroke and with existing comorbidities, healthcare providers should come up with one holistic care plan for the patient that addresses the most pressing health issue first. You should also take a look at our Event Marketing Plan
After which, goals or desired outcomes are set for each priority. This means writing down what healthcare professionals hope to achieve with the interventions implemented to address patient’s concerns and nursing diagnoses. Having goals also provide direction in the intervention and treatment planning as well as serve as criteria during evaluation of the patient’s health progress. You should also take a look at our Migration Plan
Step 4: Nursing Intervention and Rationale of the Treatment
Nursing interventions are the nursing orders which include the activities and actions that nurses have to perform to achieve the set goals for the patient. In other words, these are the treatments that will be given or provided to the patient to address their health problems. It includes a checklist of the activities on how nurses will take care of the patient. You should also take a look at our Action Plan
As an evidence-based plan, documentation of treatment implementation is required. That’s why it is important that nurses monitor the patient’s health closely and document it in their health record. This part of the plan is also dynamic and will be updated as the patient’s health conditions change or improve and will be the basis if the patient is okay to be discharged. You should also take a look at our SPA And Salon Business Plan
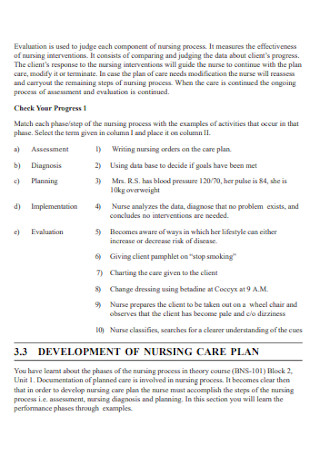
Step 5: Evaluation of the Executed Care Plan
Aside from implementing the care plan all throughout the patient’s hospitalization, their health status should be monitored and evaluated based on the goals set. Results of the evaluation will determine the effectiveness of the intervention and care being provided to the patient and if the NANDA diagnosis needs to be modified or changed, or if the treatment plan has been completed and the patient is ready to go home. You should also take a look at our Nursing Research Proposal
Importance of Nurse Care Plans
Writing a nursing care plan isn’t just for compliance. It is an important document for patient care and is used by many healthcare professionals involved in the treatment of patient’s health issues. The following are the purposes and importance of a nurse care plan:
- Define roles. The care plan helps establish the roles and responsibilities of each healthcare provider. It identifies the unique roles of nurses in attending for the overall well-being of the patient without relying on the physician’s orders all the time.
- Gives direction for the overall patient care. It engages the nurses’ critical thinking for every client that they have and develops interventions that are tailored to the specific needs of the patient.
- Ensures continuity of care. With presence of a care plan, nurses from different shifts, floors, or departments can refer to it. Having a care plan will ensure that the same care and type of intervention is provided to the patient.
- Documentation. Nurses record all of the findings from their observations and monitoring, as well as actions carried out, instructions that the client or family members require. If actions and care are not recorded, there is no evidence that they were carried out.
- Serves as a guide for proper staff assignment. The care plan can also be used as a reference to the type of nursing skills that the patient needs. Having this on hand can help determine the right staff with particular and precise skills to address patient needs.
- Guide for reimbursement. Medical records are also included in the care plan. Insurance companies also use this to determine what they will pay and how much they will pay in relation to the hospital care that the patient received.
- Involves clients. Although it may seem that the care plan is only for nurses and other healthcare workers, this also benefits the patient as they get involved in their own treatment and care.
Different types of Care Plans
There are a vast variety of diseases out there that people may or may not contract in their lifetime. But whatever that may be, there is a care plan for that. Various diseases and health conditions are grouped together and are segmented per category such as:
- Basic Nursing and General Care Plans which are examples of miscellaneous nursing care plans that do not fit other categories such as Oncology Nursing, Hospice or Palliative Care, and Geriatric Nursing, among others.
- Surgery and Perioperative Care Plans are plans that involve surgical procedures and interventions.
- Maternal and Newborn Care Plans refer to the care of a pregnant mother and her infant and is closely related to maternity and obstetric nursing.
- Pediatric Nursing Care Plan refers to those plans for pediatric cases, conditions, and diseases like Hydrocephalus, Cerebral Palsy, Croup Syndrome, Child Abuse, Meningitis, among others.
- Mental Health and Psychiatric Care Plans are for mental health and psychiatric nursing. Some examples include alcohol withdrawal, anxiety and panic disorder, major depression, personality disorder, sexual assault, and others. You should also take a look at our Best Marketing Plan
Is there a specific care plan format to follow?
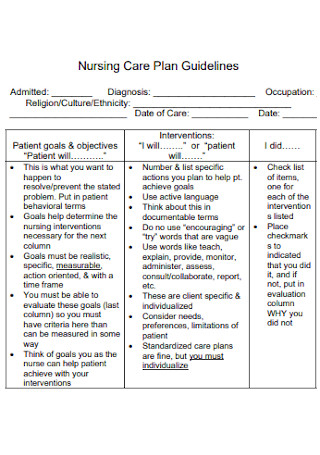
There is no one particular format to follow when it comes to care plans. As long as it contains all of the four components such as the problem as defined in the nursing diagnosis, goals set or the expected and desired outcomes, nursing interventions agreed upon by all healthcare providers involved, and evaluation of the success of the treatment or interventions. You should also take a look at our School Business Plan
What are other considerations in writing a care plan?
Aside from the main elements of a care plan and physician’s orders, other considerations in writing one include: Patient’s choice and preferences and their willingness to participate and change Include small manageable steps that the patient can easily carryout Establish who is responsible to the patient’s care plan and use layman’s language Set realistic goals and objectives to measure success to keep patients motivated. You should also take a look at our Student Lesson Plan
Are nursing interventions the same as physician interventions?
No. They are not the same. Nursing interventions do not necessarily require doctor’s orders such as reposition the patient or teaching them breathing techniques after surgery. Physician interventions, on the other hand, are carried out by the nurses such as medication administration and monitoring of certain patient behavior or output like urine and stool. You should also take a look at our Restaurant Business Plan
Can nurses question the physician’s intervention orders?
Yes. Nurses are liable for all interventions that they carry out so they should ask and question any interventions that they think are inappropriate or will not work considering the patient’s health conditions. You should also take a look at our One Page Business Plan
What are some examples of nursing care plans?
Each diagnosis has a standardized care plan but it can be adjusted based on the patient’s needs and current medical condition. There are care plans specifically for pain, cardiovascular and respiratory diseases, and cancer. Patient’s lifestyles, beliefs, and values are also taken into consideration, so care plans per patient vary. You should also take a look at our Transportation Business Plan
What Are the 5 Components of a Nursing Care Plan?
A comprehensive Nursing Care Plan includes several key components to ensure effective patient care. These components are:
- Assessment: Collecting comprehensive data about the patient’s health status.
- Diagnosis: Identifying health problems based on the assessment data.
- Planning: Setting measurable and achievable goals for patient care.
- Implementation: Executing the nursing interventions outlined in the plan.
- Evaluation: Assessing the effectiveness of the interventions and adjusting the plan as needed. You should also take a look at our Strategic Plan
How Do You Write a Nursing Care Plan?
Writing a Nursing Care Plan involves a systematic approach to address patient needs and ensure quality care. Follow these steps:
- Conduct an Assessment: Gather detailed information about the patient’s health through observation, interviews, and physical exams.
- Formulate Nursing Diagnoses: Analyze the assessment data to identify the patient’s health problems.
- Set Goals and Outcomes: Develop specific, measurable, achievable, relevant, and time-bound goals for patient care.
- Develop Interventions: Plan nursing actions to achieve the set goals.
- Implement and Evaluate: Carry out the interventions and regularly evaluate the patient’s progress, akin to reviewing a Business Plan.
What Is the Purpose of a Nursing Care Plan?
A Nursing Care Plan serves multiple essential purposes in healthcare:
- Provides Direction: Guides nurses in delivering consistent and effective care.
- Facilitates Communication: Enhances communication among healthcare team members.
- Ensures Continuity of Care: Helps in maintaining ongoing and coordinated care.
- Promotes Accountability: Documents nursing interventions and outcomes.
- Improves Patient Outcomes: Focuses on achieving specific health goals, similar to setting objectives in a School Action Plan.
What Is Included in a Nursing Plan?
A Nursing Plan encompasses various elements to ensure comprehensive patient care. These elements include:
- Patient Information: Basic details like name, age, and medical history.
- Nursing Diagnoses: Statements of the patient’s health problems.
- Goals and Expected Outcomes: Specific targets for patient health improvements.
- Nursing Interventions: Actions and strategies to achieve the goals.
- Evaluation Methods: Criteria to assess the effectiveness of the interventions, akin to components of an Agriculture Business Plan.
What Are the 5 Steps of the Nursing Care Plan?
The nursing care plan process involves five crucial steps to ensure systematic and effective patient care. These steps are:
- Assessment: Gather comprehensive patient data.
- Diagnosis: Identify patient health problems based on assessment data.
- Planning: Set specific, measurable goals and plan interventions.
- Implementation: Execute the planned interventions.
- Evaluation: Assess the outcomes and adjust the plan as necessary, similar to reviewing and adjusting a Workout Plan.
How to Develop a Care Plan?
To develop a care plan, assess the patient, identify problems, set goals, plan interventions, and evaluate outcomes, similar to creating a Work Plan.
What Are the Two Types of Nursing Care Plan?
The two types of nursing care plans are individualized care plans, tailored to specific patients, and standardized care plans, which are generic and used for common conditions, similar to a Study Plan.
What Is a Patient’s Care Plan?
A patient’s care plan outlines specific healthcare goals, interventions, and evaluations for an individual, ensuring coordinated and comprehensive care, akin to a Community Action Plan.
What Is the Priority of a Nursing Care Plan?
The priority of a nursing care plan is to address the most critical health issues first, ensuring patient safety and effective treatment, much like a Boutique Business Plan focuses on key priorities.
How to Show Compassion as a Nurse?
Show compassion by actively listening, providing emotional support, showing empathy, being patient, and maintaining a positive attitude, similar to fostering a supportive environment in a Fast Food Business Plan.
What Are the Nursing Notes in a Care Plan?
Nursing notes in a care plan document patient assessments, interventions, responses, and progress, ensuring comprehensive and continuous care, much like detailed entries in a Digital Marketing Plan.
How to Develop a Care Plan?
To develop a care plan, assess the patient’s needs, set specific goals, plan interventions, implement actions, and evaluate progress, similar to a strategic School Development Plan
In conclusion, mastering the creation of a Nursing Care Plan is essential for effective patient care and professional nursing practice. With our guide, you have learned how to draft detailed samples, forms, and letters, ensuring your care plans are comprehensive and impactful. Utilizing the provided templates and tips, you can streamline your care planning process and enhance the quality of your nursing interventions. For more detailed examples and templates, visit Nursing Project Proposal.